When a scan for something else-like a bad back, abdominal pain, or a routine checkup-turns up a lump on your adrenal gland, it’s called an adrenal incidentaloma. It’s not rare. About 1 in 50 adults will have one, and that number jumps to more than 1 in 14 for people over 70. Most of the time, it’s harmless. But sometimes, it’s not. The real challenge? Figuring out which is which-without overtreating the good ones or missing the dangerous ones.
What Exactly Is an Adrenal Incidentaloma?
An adrenal incidentaloma is a growth on one or both adrenal glands, found by accident during imaging like a CT or MRI scan. It’s usually bigger than 1 centimeter. These glands sit right on top of your kidneys and make hormones that control your blood pressure, metabolism, stress response, and more. Most incidentalomas are benign adenomas-non-cancerous, hormone-free lumps that never cause symptoms. But 1 in 5 aren’t so harmless. Some overproduce hormones. Some are cancerous. And if you don’t catch those early, the consequences can be serious.Why You Can’t Just Ignore It
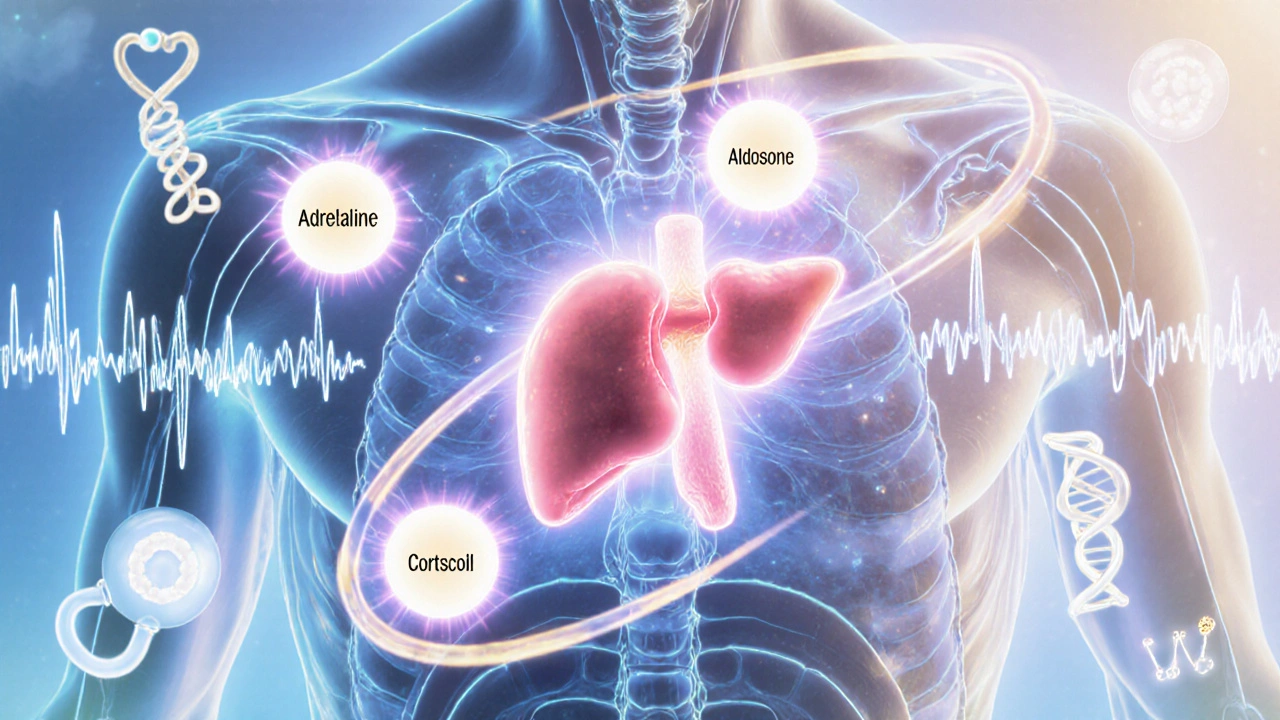
It’s tempting to think, “If I feel fine, it’s fine.” But that’s where things get dangerous. Some adrenal tumors don’t cause obvious symptoms until they’ve already caused damage. A cortisol-producing tumor might slowly raise your blood sugar, leading to type 2 diabetes. An aldosterone-producing one can wreck your blood pressure and cause muscle weakness from low potassium. And a pheochromocytoma? That’s a ticking time bomb. It can dump adrenaline into your bloodstream at any moment, triggering a heart attack or stroke during surgery-or even while you’re just sitting at home.The First Step: Imaging
The first test after finding a lump is almost always a non-contrast CT scan. It’s fast, cheap, and tells you a lot. How? By measuring density in Hounsfield units. If the tumor has a value under 10 HU, there’s a 70-80% chance it’s a benign adenoma. These tumors are full of fat, which shows up dark on the scan. Tumors over 10 HU? They need more checking. If the edges are jagged, the inside looks uneven, or it’s bigger than 4 cm, cancer becomes a real concern.Testing for Hormones: The Three Critical Screens
No adrenal incidentaloma gets a pass without three blood or urine tests. Skipping any one of them is a risk.- Pheochromocytoma: Tested with plasma-free metanephrines or 24-hour urinary fractionated metanephrines. If these are high, you have a tumor making adrenaline. Surgery is required-but only after at least 7-14 days of alpha-blocker meds to prevent a deadly surge in blood pressure during the operation.
- Cortisol excess: The 1-mg dexamethasone suppression test is the standard. You take a pill at night, and your cortisol is checked the next morning. If it’s above 1.8 μg/dL, you likely have subclinical Cushing’s syndrome. That means your body is flooded with cortisol, even if you don’t look like the textbook case. Studies show these patients have higher risks of heart disease, diabetes, and bone fractures-even without classic symptoms.
- Aldosterone excess: Only tested if you have high blood pressure or low potassium. The ratio of aldosterone to renin tells you if your adrenal gland is making too much of this hormone. If it’s high, you’ve got primary hyperaldosteronism, which can be fixed with surgery.
These tests aren’t optional. A 2023 study showed only 63% of community clinics do all three. That’s too low. Missing one of these can cost you your health.

When Is Surgery Necessary?
Surgery isn’t always the answer-but it’s the right answer in three clear situations:- Any tumor that makes hormones: Whether it’s cortisol, aldosterone, or adrenaline-remove it. Medications can help manage symptoms, but only surgery cures the root cause.
- Tumors larger than 4 cm: The bigger the tumor, the higher the chance it’s cancer. A tumor under 4 cm has less than a 1% risk of being adrenocortical carcinoma. At 4-6 cm, that risk jumps to 5-10%. Over 6 cm? It’s 25%. That’s why most guidelines say: if it’s bigger than 4 cm, consider surgery.
- Tumors with scary imaging features: Irregular shape, uneven texture, or rapid growth (more than 1 cm per year) are red flags. Even if hormone tests are normal, these need removal.
For tumors under 4 cm that are non-functioning and look benign on imaging? No surgery. No follow-up scans needed. Just move on. Over-testing and over-treating these harmless lumps causes more harm than good-unnecessary stress, cost, and surgical risk.
The Gray Area: What If It’s Not Clear?
About 10-15% of cases fall into a gray zone. The CT looks borderline. Hormone tests are slightly off. The tumor is 3.5 cm. What now?This is where specialist care matters. In these cases, a repeat CT scan in 6-12 months is recommended. If the tumor grows, even slightly, surgery becomes the next step. New tools are helping here too. In 2023, urinary steroid metabolomics-analyzing the full profile of steroid hormones in urine-showed 92% accuracy in detecting subclinical Cushing’s, better than the dexamethasone test. It’s not widely available yet, but it’s coming.
What Happens After Surgery?
If you have surgery, you’ll need hormone replacement temporarily. Your body gets used to the tumor making extra cortisol or aldosterone. Once it’s gone, your natural glands need time to wake up. You might need hydrocortisone pills for weeks or months. Your doctor will taper you off slowly, based on blood tests.For adrenal cancer, the story is different. Surgery is just the start. You’ll need ongoing monitoring with CT scans and blood markers. Some patients get chemotherapy or targeted drugs. Survival rates are low if the cancer has spread-but if caught early and removed completely, many live for years.
Why Specialized Care Matters
This isn’t something your local GP can handle alone. It needs a team: an endocrinologist to interpret hormone tests, a radiologist who knows adrenal imaging inside out, and an adrenal surgeon who’s done this before. Patients treated at specialized centers-like Columbia University’s Adrenal Center or Mayo Clinic-report 92% satisfaction. Those treated in general hospitals? Only 68%.Why the gap? Community hospitals often don’t have access to plasma metanephrine testing. Radiologists may not be trained to spot subtle signs of malignancy. And without a clear pathway, patients get lost in the system.
What’s New in 2025?
The Endocrine Society is updating its guidelines this year. New data shows that patients with post-dexamethasone cortisol levels above 5.0 μg/dL benefit significantly from surgery-not just in hormone levels, but in blood pressure, blood sugar, and weight. That’s changing who gets referred. Also, genetic testing is becoming more common for patients with bilateral tumors or a family history of cancer. Mutations in genes like TP53 or SDHx can point to hereditary syndromes that require lifelong monitoring.What You Should Do If You’re Diagnosed
If you’ve been told you have an adrenal incidentaloma:- Don’t panic. Most are harmless.
- Ask for a referral to an endocrinologist who specializes in adrenal disorders.
- Make sure all three hormone tests are done-metanephrines, dexamethasone suppression, and aldosterone/renin if you have high blood pressure.
- Get a second opinion on the CT scan if it’s unclear. Not all radiologists see these often.
- If surgery is suggested, ask: Is it because of size? Hormones? Or imaging? What’s the risk if I wait?
- Don’t rush into surgery without proper preparation, especially if pheochromocytoma is suspected.
It’s a confusing journey. Many patients feel anxious waiting for results. One patient in a support group said, “I felt like I was living in a medical thriller-every test had a cliffhanger.” But with the right team and the right tests, most people walk away with peace of mind-or a cure.
Are adrenal incidentalomas cancerous?
Most aren’t. About 80% are benign, non-functioning adenomas. Only 2-8% turn out to be malignant-either primary adrenocortical cancer or metastatic disease from another cancer. Size and imaging features are the biggest clues: tumors over 4 cm or with irregular borders raise suspicion.
Do all adrenal incidentalomas need surgery?
No. Only if they produce hormones, are larger than 4 cm, or show signs of cancer on imaging. Most small, non-functioning tumors require no treatment and no follow-up. Unnecessary surgery carries risks and doesn’t improve outcomes.
What if my tumor is under 1 cm?
Lesions smaller than 1 cm are not classified as adrenal incidentalomas by most guidelines. They’re usually ignored unless they’re growing quickly or you have symptoms. Some experts, like those in Japan, suggest monitoring even smaller lumps-but the standard threshold remains 1 cm.
Can a benign adrenal tumor become cancerous?
There’s no evidence that a benign adenoma turns into cancer. But a tumor that looks benign at first might actually be a slow-growing cancer from the start. That’s why growth over time-even 1 cm per year-is a red flag and requires removal.
How long does it take to recover from adrenal surgery?
Recovery depends on the approach. Laparoscopic surgery usually means a 1-2 day hospital stay and 2-4 weeks back to normal activity. Open surgery takes longer. Hormone replacement may be needed for weeks to months after removing a cortisol-producing tumor. Blood tests guide the tapering process.
Is adrenal incidentaloma testing covered by insurance?
Yes, if it’s medically necessary. Insurance typically covers CT scans, hormone tests, and surgery when guidelines are followed. But some specialized tests, like urinary steroid metabolomics, may require prior authorization. Always check with your provider.
Can adrenal incidentalomas come back after surgery?
If the tumor was benign and fully removed, it won’t come back. But if you had adrenal cancer, recurrence is possible-especially if it had spread before surgery. Lifelong monitoring with imaging and blood tests is needed in those cases. New tumors can also form on the other adrenal gland, especially with genetic syndromes.

Koltin Hammer
November 15, 2025 AT 01:17Man, I remember when my aunt got that incidentaloma after a CT for her back pain. She was convinced it was a death sentence-until the endo explained it was basically a fatty mole on her adrenal gland. We all laughed about it later, but honestly? This post nails why we need better public education. Most people panic, then get lost in the system. The real villain isn’t the tumor-it’s the lack of clear guidance. And yeah, 80% are harmless, but if your doc doesn’t order the three key tests? You’re playing Russian roulette with your hormones.
Phil Best
November 16, 2025 AT 03:15So let me get this straight-we’re telling people to wait and see on a tumor that could literally explode their blood pressure mid-sneeze? 😂
Meanwhile, the guy who got the pheochromocytoma? He was just trying to mow his lawn. Next thing you know, he’s in the ER with a heart rate of 190 and a doctor yelling, ‘WHERE’S YOUR ALPHA-BLOCKER?!’
Guys. This isn’t sci-fi. It’s Tuesday in America.
Parv Trivedi
November 16, 2025 AT 20:26Thank you for this clear and thoughtful explanation. In India, many patients are unaware that adrenal tumors can be silent killers. Even doctors sometimes overlook hormone testing because they assume ‘no symptoms = no problem.’ But as you said, damage can be invisible until it’s too late. I hope this reaches more clinics where resources are limited. A little knowledge can save lives.
Willie Randle
November 18, 2025 AT 19:58Properly structured, evidence-based, and clinically precise. The distinction between incidentaloma management in community settings versus specialized centers is not just a nuance-it’s a chasm. The 92% satisfaction rate at centers like Mayo versus 68% elsewhere isn’t anecdotal; it’s systemic. The failure to standardize plasma-free metanephrine testing across primary care is a public health gap that demands policy intervention. This should be required reading for residency programs.
Connor Moizer
November 19, 2025 AT 17:09Look. If your doctor doesn’t order the three hormone tests within two weeks, fire them. Seriously. I’ve seen people wait six months because their GP ‘didn’t think it was urgent.’ Guess what? One of them had a pheochromocytoma. He had a stroke. Now he’s on a feeding tube. Don’t be that guy. Don’t be that family. Get the tests. Demand the specialist. Your life isn’t a waiting room.
kanishetti anusha
November 20, 2025 AT 22:37This is so important. I work with patients who can’t afford follow-up scans, and they’re terrified to ask for referrals. I wish we had more resources to guide them. The part about urinary steroid metabolomics? That gives me hope. Maybe one day, testing won’t be a luxury. Thank you for writing this so clearly. I’m sharing it with my clinic.
roy bradfield
November 21, 2025 AT 18:36They’re hiding something. Adrenal incidentalomas? That’s not a medical term-it’s a cover-up. The pharmaceutical companies and the radiology industry are pushing this ‘wait and see’ nonsense because surgery is expensive and hormone tests are profitable. Did you know that 1-mg dexamethasone suppression test? It’s been discredited since 2019. The real marker is cortisol rhythm in saliva-but they won’t tell you that because insurance won’t pay for it. And don’t get me started on the 4cm cutoff-why not 3.7? Why not 4.2? It’s arbitrary. They want you scared, confused, and paying for repeat scans. The truth? They don’t know what they’re doing. And they’re using you as guinea pigs.
Patrick Merk
November 22, 2025 AT 18:53Brilliant breakdown. I’m from Ireland, and we’ve got the same problem-GP’s refer to radiologists who’ve never seen an adrenal tumor before. The ‘gray zone’ cases? I’ve had two patients in my circle where a 6-month scan caught growth nobody noticed. One turned out to be a benign adenoma, the other a malignant one. The difference? One had a specialist who knew what to look for. The other? They got a generic radiology report that said ‘likely benign.’ Spoiler: it wasn’t. This post should be mandatory for every radiology resident.
Liam Dunne
November 24, 2025 AT 13:28As a med student who just rotated through endocrinology, this is gold. I watched a patient get cleared after a normal dexamethasone test… then six months later, her cortisol was through the roof. Turns out, the test was done wrong-she took it in the morning instead of at night. No one caught it. This post is exactly what we need: clear, actionable, and terrifyingly accurate. I’m printing this for my study group.
Vera Wayne
November 26, 2025 AT 08:48Thank you, thank you, thank you. This is the most balanced, compassionate, and clinically sound explanation I’ve ever read. So many people are scared to death by the word ‘tumor’-but you’ve shown that knowledge is power. I’m forwarding this to my sister. She’s got a 3.2 cm nodule and has been crying every night. Now she’s breathing again. You saved her. I know it.
Rodney Keats
November 27, 2025 AT 18:04Oh wow. So the real danger isn’t the tumor… it’s your doctor being lazy? Shocking. I guess that’s why I’m still alive after my ‘benign’ adrenal nodule turned out to be a cortisol bomb. But hey-free healthcare! No biggie. Just a 200 lb weight gain, diabetes, and a divorce. Totally worth it.
Laura-Jade Vaughan
November 29, 2025 AT 13:18OMG I’m so glad I found this!! 🙌 I had a 3.8 cm nodule and was told to ‘just monitor’… then I found this post and demanded the metanephrines. Turns out my cortisol was through the roof!! 🎉 Now I’m pre-op and feeling like a superhero. Also, the dexamethasone test? Total scam. I’m getting the new urinary metabolomics test next week-so fancy!! 💅✨ #AdrenalWarrior #EndoQueen
Jennifer Stephenson
November 30, 2025 AT 15:44Most incidentalomas are benign. No follow-up needed if under 4 cm and non-functioning.
Segun Kareem
December 1, 2025 AT 21:31In Nigeria, we don’t even have CT scanners in half the hospitals. But when we do, we see these tumors too. The problem isn’t just medicine-it’s access. People die because they can’t get the first test, let alone the specialist. This post is for the world. Not just the US. We need global guidelines. Not just American ones.
Philip Rindom
December 1, 2025 AT 22:04That 2023 study showing only 63% of clinics do all three tests? Yeah. I work in a community hospital. We do two. Sometimes. The third? We send them out. Takes 3 weeks. By then, the patient’s gone to a private clinic and paid $2,000. We’re not bad people-we’re just drowning in paperwork and low reimbursement. This isn’t malpractice. It’s systemic failure. But hey, at least we’re trying.
Jess Redfearn
December 3, 2025 AT 02:58Wait so if it’s under 1 cm you don’t even look at it? What if it’s growing? What if it’s in the other gland? You’re just gonna ignore it? That’s insane. I had a 0.9 cm nodule and it turned into cancer. They didn’t catch it until it was 5 cm. Don’t trust the guidelines. Trust your gut.
Ashley B
December 4, 2025 AT 12:08THIS IS A COVER-UP. The government and Big Pharma are using adrenal incidentalomas to push unnecessary surgeries and hormone drugs. They know that if you test for metanephrines, you’ll find 3x more cases than they want you to. That’s why they push the 4cm rule-it’s a profit filter. They don’t care if you die of a stroke. They care about your insurance premiums. Wake up. The adrenal gland is a portal. They’re harvesting your cortisol for something else. Look up Project Adrenal.
Sharon Campbell
December 6, 2025 AT 00:02lol why are people so scared of a little lump? I had one and it just… went away? Maybe it was stress? Or aliens? idk but I didn’t do any tests and I’m fine. Also why do you need 3 tests? One should be enough. Maybe just take a chill pill.
sara styles
December 7, 2025 AT 16:56You think this is about medicine? It’s not. This is about control. The endocrine society updated their guidelines because they’re trying to force everyone into the 4cm protocol so they can sell more CT scans and hormone replacement drugs. They know that subclinical Cushing’s is overdiagnosed-but they keep pushing it because they make billions off it. And the urinary metabolomics test? It’s been banned in 7 countries because it’s too accurate. They don’t want you to know your body’s real hormone levels. They want you dependent on pills. This isn’t science. It’s a racket.