Warfarin-Antibiotic Interaction Checker
Check Your Antibiotic Risk
This tool helps you determine if your antibiotic interacts with warfarin and what level of risk you should be aware of. Always consult your doctor before making changes to your medication.
Antibiotic Risk Assessment
Key Timing Information:
What You Should Do:
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance - sometimes with life-threatening results. This isn't just a theoretical risk. In the U.S., nearly one in three warfarin-related hospital visits involves an antibiotic. The problem? Antibiotics don't just kill bacteria. They also mess with your body's ability to control clotting. And if you're not watching your INR closely, you could bleed internally without warning.
Why Antibiotics and Warfarin Don't Mix
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It's a tightrope walk: too little, and you clot; too much, and you bleed. Your INR tells you where you stand. For most people, the target is 2.0 to 3.0. Once it hits 4.0 or higher, your risk of major bleeding jumps four to eight times. Antibiotics interfere in two main ways. First, they kill off the good bacteria in your gut that make vitamin K. Second, some antibiotics slow down the liver enzymes (CYP2C9) that break down warfarin. That means warfarin builds up in your blood - and your INR climbs fast. This isn't random. Certain antibiotics are far more dangerous than others. Ciprofloxacin, Bactrim, and erythromycin are high-risk. Amoxicillin? Less so. But even "safe" ones can cause trouble if you're older, have kidney issues, or are on a high warfarin dose.High-Risk Antibiotics That Spike INR
Not all antibiotics are created equal when it comes to warfarin. Here’s what the data shows:- Ciprofloxacin and levofloxacin (fluoroquinolones): These are the worst offenders. Studies show INR can jump from 2.5 to 4.1 within a week. Bleeding risk increases over two-fold.
- Bactrim (sulfamethoxazole/trimethoprim): Causes INR spikes of 1.8 units on average. One study found 1 in 5 patients needed a warfarin dose reduction.
- Erythromycin: Strongly inhibits liver enzymes. Bleeding risk rises 2.3 times.
- Amoxicillin/clavulanate: Doesn’t affect liver enzymes, but wipes out gut bacteria. INR rises about 1.2 units - enough to matter.
- Cefotetan and cefoperazone (cephalosporins): These have a special side chain that blocks vitamin K. INR can climb 1.5 to 2.2 units.
- Rifampin: The opposite problem. It speeds up warfarin breakdown. INR drops below 1.5 - putting you at risk for clots.
On the other hand, azithromycin, nitrofurantoin, and fosfomycin have minimal interaction. But don’t assume anything is "safe" without checking.
When Do INR Spikes Happen? Timing Matters
The timing of the spike tells you what’s going on.- 2 to 3 days after starting antibiotics: This points to liver enzyme inhibition. Fluoroquinolones and macrolides act fast. Your INR can rise quickly - often before you even feel symptoms.
- 5 to 7 days after starting: This is gut bacteria depletion. Cephalosporins and penicillins take longer. You might feel fine for a week, then suddenly start bruising easily.
- After stopping the antibiotic: The danger doesn’t end when you finish the pill. Gut bacteria can take 7 to 10 days to recover. INR may stay high or even climb further. Many patients bleed after their antibiotic course ends.
This is why checking your INR only once during antibiotic therapy isn’t enough. You need to monitor before, during, and after.
What Doctors Should Do - And What You Should Ask For
The American College of Chest Physicians says this clearly: Check your INR within 72 hours of starting any antibiotic, then twice a week until the antibiotic is done - and again after. But in real life? Many patients get no extra testing. A 2023 GoodRx analysis found that 42% of warfarin-related ER visits happened because the patient didn’t get their INR checked during antibiotic treatment. Here’s what you need to ask:- "Is this antibiotic safe with warfarin?"
- "Will you check my INR before I start and again in 3 days?"
- "Should I hold off on my next warfarin dose?"
- "When should I check my INR after I finish the antibiotics?"
Some clinics now use pharmacist-led warfarin management. Studies show this cuts bleeding risk by 37%. If your doctor doesn’t offer it, ask why.
What to Do If Your INR Goes Too High
If your INR is between 3.1 and 4.0 and you have no bleeding, your doctor might just skip your next warfarin dose and recheck in 2-3 days. But if your INR is above 4.0 - especially above 5.0 - you’re in danger. Here’s what happens next:- INR 4.0-5.0: Stop warfarin. Give vitamin K (1-2.5 mg orally). Recheck INR in 24 hours.
- INR 5.0-9.0: Stop warfarin. Give 2.5-5 mg vitamin K. Consider fresh frozen plasma if you’re actively bleeding.
- INR >9.0: Emergency treatment. Vitamin K, plasma, and hospitalization are likely needed.
Don’t wait for symptoms. If your INR is high, bleeding can happen suddenly - a nosebleed that won’t stop, dark stools, or blood in your urine. These aren’t "minor" issues. They’re red flags.
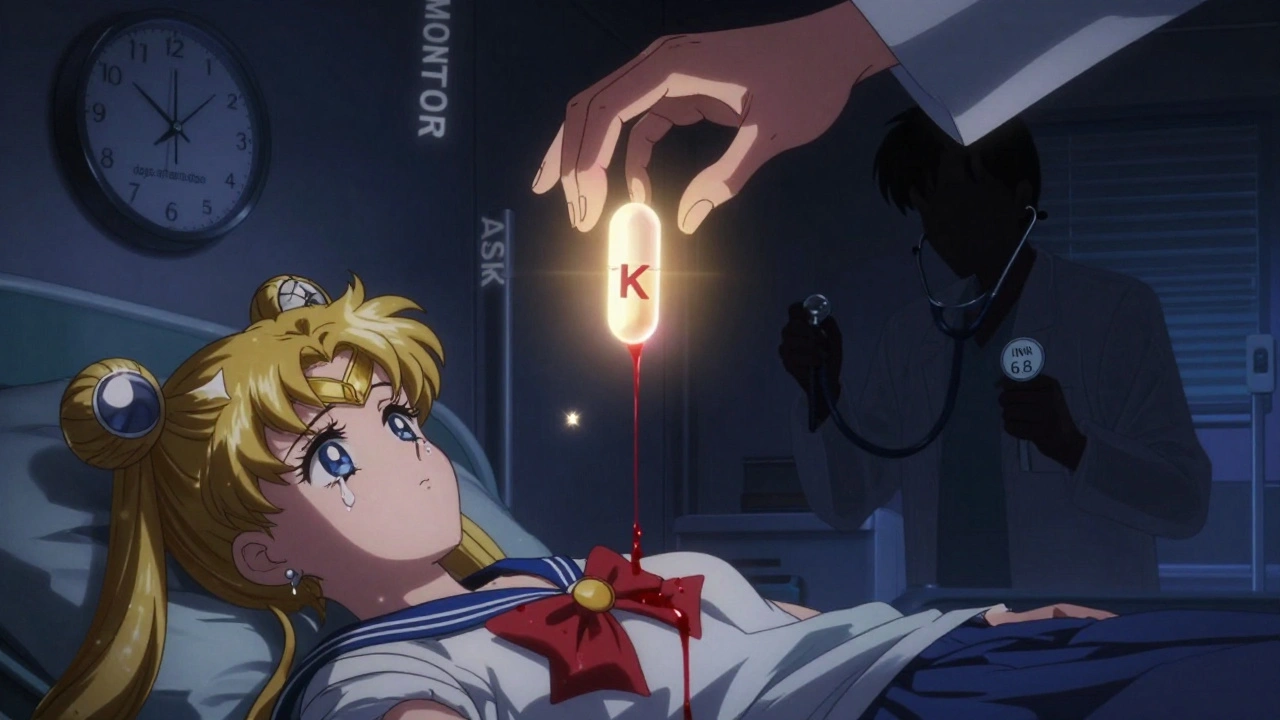
Real-Life Scenarios - What Goes Wrong
Take Maria, 72, on warfarin for atrial fibrillation. Her INR is steady at 2.6. She gets a UTI and is prescribed ciprofloxacin. Her doctor doesn’t mention warfarin. Three days later, she trips and falls, develops a huge bruise on her thigh, and feels dizzy. She goes to the ER. Her INR is 6.8. She needs vitamin K and plasma. She spends three days in the hospital. Or James, 68, on warfarin after a knee replacement. He gets a sinus infection and is given amoxicillin/clavulanate. He feels fine. He finishes the antibiotics. A week later, he notices blood in his urine. His INR is 5.2. The infection is gone, but his gut bacteria haven’t recovered yet. These aren’t rare. They’re predictable - and preventable.What You Can Do Right Now
If you’re on warfarin:- Keep a log of every antibiotic you take - name, dose, start and end date.
- Always tell your pharmacist and doctor you’re on warfarin - even for a simple ear infection.
- Ask for an INR check before starting any new antibiotic.
- Know the signs of bleeding: unusual bruising, red or black stools, vomiting blood, severe headaches, sudden weakness.
- If you’re prescribed an antibiotic, schedule your next INR test before you leave the clinic.
- Don’t skip your warfarin dose unless told to - even if your INR is high. Your doctor will adjust it.
There’s no magic pill that makes this interaction go away. But you can control the outcome - by being informed, asking questions, and demanding monitoring.
What’s Changing in 2025
New research is making things better. In 2023, the WARF-GEN trial showed that patients who got genetic testing for CYP2C9 variants had 41% fewer INR spikes during antibiotic use. If you’ve been on warfarin for years, ask if genetic testing is right for you. Also, newer antibiotics like tedizolid (used for skin infections) show almost no interaction with warfarin. Your doctor may be able to choose one that’s safer. Electronic alerts in hospitals help - but only if they’re paired with real clinical guidance. A 2019 study found alerts alone reduced errors by just 7%. Add a pharmacist, and it jumps to 22%. The bottom line? We’re getting smarter. But you still have to be your own advocate.Can I take azithromycin with warfarin?
Yes, azithromycin is one of the safest antibiotics to take with warfarin. It doesn’t significantly affect liver enzymes or gut bacteria. Studies show only a 1.2-fold increase in bleeding risk - which is close to normal. Still, it’s wise to check your INR before and after taking it, especially if you’re older or have other health issues.
How long should I wait to check my INR after stopping an antibiotic?
Check your INR within 72 hours after finishing the antibiotic - even if you feel fine. For antibiotics that kill gut bacteria (like amoxicillin or cefotetan), the INR may keep rising for up to 10 days after stopping. Don’t assume the danger is over just because the pills are done.
Do all antibiotics affect warfarin?
Almost all do - but to different degrees. Fluoroquinolones, Bactrim, and some cephalosporins are high-risk. Azithromycin, nitrofurantoin, and fosfomycin are low-risk. But no antibiotic is completely risk-free. Always assume interaction until proven otherwise.
Can vitamin K supplements prevent INR spikes?
No. Taking extra vitamin K to "counteract" antibiotics is dangerous. It can make your warfarin ineffective and increase your risk of stroke or clot. Only take vitamin K if your doctor orders it for a high INR. Never self-treat.
Why does my doctor say to check my INR even if I feel fine?
Because bleeding from warfarin doesn’t always hurt. You can have a slow bleed in your brain, gut, or muscle without pain until it’s serious. INR is the only way to know your blood is too thin. Feeling fine doesn’t mean your INR is safe.


मनोज कुमार
December 2, 2025 AT 03:32Antibiotics wreck INR like a dumpster fire. Cipro? Absolute nightmare. Bactrim? Same. Docs don't give a shit until someone bleeds out. Check INR before, during, after. Or don't. Your funeral.
Joel Deang
December 3, 2025 AT 15:48OMG YES THIS!! I got cipro for a UTI and my INR went to 6.2 😱 I thought I was just tired but nooo… had to go to ER. My doc was like 'uhhh maybe check next time?' like bro I almost died. Plz ppl ask for INR checks!!
Roger Leiton
December 4, 2025 AT 22:10Really appreciate this breakdown. The timing aspect is so underdiscussed - I never realized the gut bacteria angle takes days to manifest. It’s not just the antibiotic itself, it’s the ripple effect. Also, azithromycin being safer is a game-changer for folks like me on long-term warfarin. Thanks for the clarity.
Laura Baur
December 5, 2025 AT 14:28It’s frankly criminal that this isn’t standard protocol everywhere. The fact that 42% of ER visits are preventable with a simple INR check reveals a systemic failure in primary care - a failure of accountability, of education, of basic human compassion. We treat warfarin like a magic pill, not a precision instrument. And patients pay the price with their blood, their organs, their lives. This isn’t just medical advice - it’s a moral imperative.
Jack Dao
December 6, 2025 AT 06:48Wow. So you’re telling me people who don’t read the damn article and just trust their doctor are gonna die? I mean… I guess that’s the point. But still. If you’re on warfarin and you can’t be bothered to Google drug interactions, maybe you shouldn’t be allowed to take pills. Just saying.
dave nevogt
December 8, 2025 AT 05:12I’ve been on warfarin for 12 years after a PE. I’ve had two INR spikes from antibiotics - one from amoxicillin/clavulanate after a sinus infection. I felt fine. No bruising, no pain. Then I woke up with blood in my urine. It wasn’t dramatic. It was quiet. That’s the scariest part. The body doesn’t scream before it collapses. Monitoring isn’t paranoia. It’s survival. I wish more people understood that.
ATUL BHARDWAJ
December 8, 2025 AT 09:59INR check before antibiotic. Simple. Done.
Steve World Shopping
December 9, 2025 AT 01:41Fluoroquinolones are the new black plague. Cipro = warfarin suicide. Bactrim = INR grenade. Cephalosporins? Quiet killers. The pharmacokinetics are well-documented. If your provider doesn’t know this, they’re not fit to prescribe. This is not opinion. This is clinical fact. Educate yourself or die.
Rebecca M.
December 10, 2025 AT 04:30Oh sweetie. You mean that time your doctor gave you cipro and didn’t check your INR… and then you cried in the ER because you ‘didn’t know’? Honey. You’re not a victim. You’re just… a person who didn’t read the pamphlet. But hey, at least now you’ve got a great story for your next therapy session. 💅🩸