When you write a prescription, you’re not just choosing a medicine-you’re choosing a system. Generic prescribing means writing the International Non-proprietary Name (INN) of a drug, not its brand name. It’s not a cost-cutting trick. It’s the standard of care in most of the world, backed by decades of evidence and endorsed by every major health authority-from the WHO to the NHS and the FDA.
Why Generic Prescribing Is the Default
Generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t carry the marketing, advertising, and patent protection costs of brand-name drugs. The active ingredient? Identical. The dosage? The same. The manufacturing standards? Just as strict.
In the UK, the NHS saves around £1.3 billion every year just by prescribing generics instead of brands. Take atorvastatin: the generic version costs £2.50 a month. The brand, Lipitor? £30. Omeprazole? Generic: £1.80. Losec? £15. That’s not a small difference-it’s life-changing for patients on long-term meds.
And it’s not just about money. Studies show patients are 8-12% more likely to stick with their medication when it’s affordable. Fewer missed doses mean fewer hospital visits. One JAMA study found that switching to generics led to 15% fewer hospitalizations for chronic conditions like hypertension and diabetes.
When Brand-Name Prescribing Is Still Necessary
Generic prescribing isn’t a one-size-fits-all rule. There are exceptions-and they’re not random. They’re based on real clinical risk.
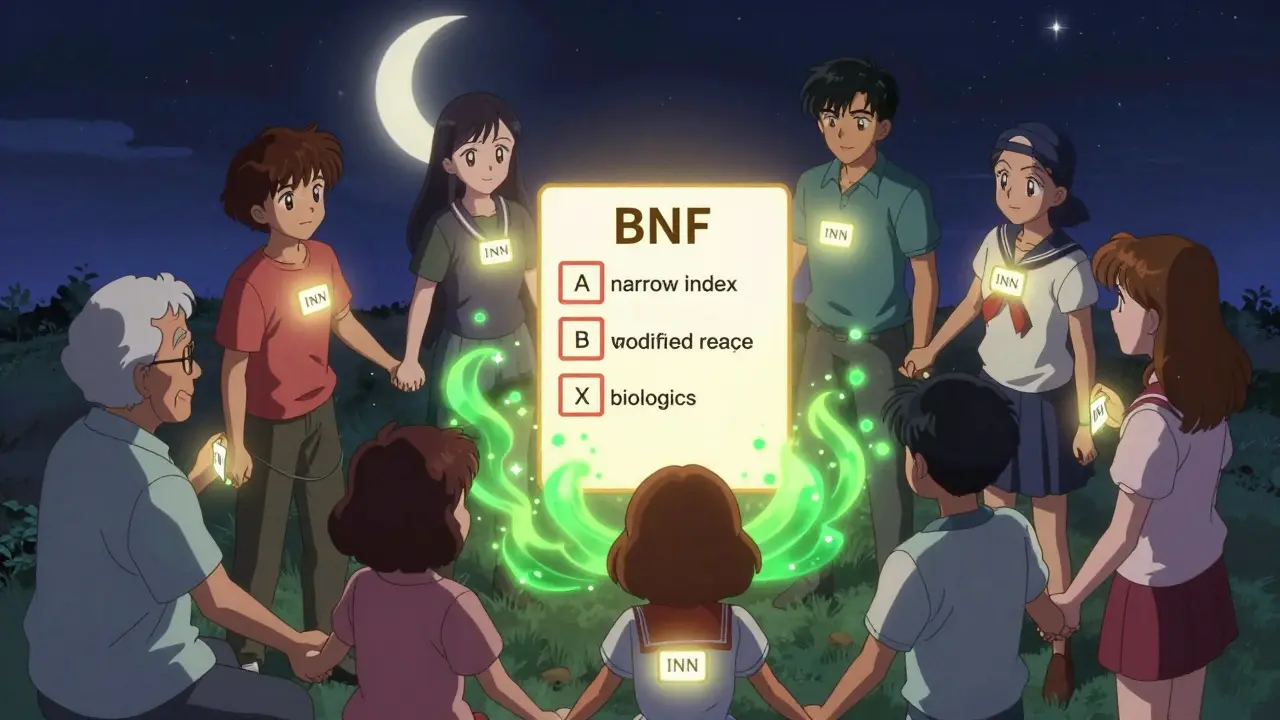
The British National Formulary (BNF) clearly defines three categories where brand-name prescribing should be the norm:
- Category 1: Narrow therapeutic index drugs-where even tiny changes in blood levels can cause harm. These include warfarin, digoxin, levothyroxine, phenytoin, and carbamazepine. For these, switching between brands-even generics from different manufacturers-can cause INR spikes, seizures, or thyroid instability.
- Category 2: Modified-release formulations-like theophylline or certain slow-release opioids. The way the drug is released matters. A generic version might release the active ingredient too fast or too slow, even if the total dose is the same.
- Category 3: Biologics and biosimilars-insulin, infliximab, adalimumab. These are complex proteins. The MHRA and FDA both require brand-name prescribing here because switching between originator and biosimilar can trigger immune reactions. Automatic substitution is not allowed.
That’s about 2% of all prescriptions. The rest? Generic is not just acceptable-it’s the best choice.
How Generic Prescribing Reduces Errors
Imagine a patient takes three different brands of the same drug: one called “Lipitor,” another “Atorvastatin Sandoz,” and a third “Atorvastatin Teva.” Now imagine a pharmacist, a nurse, or even the patient themselves gets confused. Which one is which? What’s the dose? What’s the interaction?
Generic prescribing cuts that confusion in half. One name. One standard. No brand confusion.
The Institute for Safe Medication Practices found that switching to generic prescribing reduces medication errors by 50%. Why? Because you’re not dealing with 15 different names for the same chemical. You’re dealing with one: amoxicillin, metformin, sertraline.
It’s not just safer for the patient. It’s easier for you. Less time spent checking which brand is which. Less risk of prescribing the wrong one.

What Patients Think-And How to Talk to Them
Some patients are skeptical. They’ve heard stories. They’ve seen ads. They think, “If it’s cheaper, it must be weaker.”
That’s the nocebo effect in action. A 2021 study found that when patients were told generics were inferior, 30% reported side effects or reduced effectiveness-even though the drug was identical.
But here’s the good news: when you explain it clearly, acceptance jumps from 67% to 89%.
Use this script:
“This generic version has the same active ingredient as the brand you’ve been taking. It’s been tested to work the same way. The only difference is the price-it’ll save you about £12 a month. There’s no drop in effectiveness.”
Don’t say, “It’s just a generic.” Say, “It’s the same medicine, just without the brand name.”
Patients on sertraline and levothyroxine are the most likely to raise concerns. That’s not because generics don’t work-it’s because those drugs are sensitive. But even then, most patients do just fine. One GP on Reddit with 12 years of experience said: “95% of my patients switch without issue. The 5% who don’t? We monitor them closely.”
How to Implement This in Practice
Getting to 90%+ generic prescribing isn’t hard. It’s about systems, not willpower.
NHS England’s 2023 toolkit recommends four steps:
- Audit your prescribing. Use the Prescribing Analytics Dashboard. See where you’re still prescribing brands unnecessarily.
- Know the exceptions. Keep the BNF’s three categories handy. Print them. Put them on your screen. Memorize the top 10 high-risk drugs.
- Set defaults in your e-prescribing system. Most systems let you set “generic” as the default. Turn it on.
- Track your progress. The NHS Business Services Authority tracks prescribing data monthly. See your rate go up.
Most practices hit 92-95% generic rates within six months. The remaining 5-8%? Those are the justified exceptions.
What’s Changing in 2025
The rules aren’t static. In March 2023, the MHRA updated its guidance to include complex generics like glatiramer acetate-used in multiple sclerosis-where manufacturing differences matter enough to require brand-name prescribing.
The FDA’s GDUFA III rules, rolled out in 2023, now require manufacturers to report any formulation-related adverse events. That means better post-market monitoring. Fewer surprises.
And the NHS is pushing for 92% generic prescribing by March 2024. That’s not a target-it’s a baseline. The goal is intelligent substitution: using real-world data to know which patients can switch safely, and which need brand continuity.
By 2025, 75% of small-molecule drugs will have generics. But biologics? Only 40% will have biosimilars. That’s where the next challenge lies.
Final Thought: Prescribing Generically Is Professional Responsibility
This isn’t about saving money for the NHS. It’s about saving time, reducing errors, improving adherence, and giving patients better outcomes.
The American College of Physicians says it plainly: “Clinicians should prescribe generic medications whenever possible.”
That’s not a suggestion. It’s a standard. And if you’re not doing it, you’re not just missing out on savings-you’re missing out on better care.
Start today. Check your next prescription. Is it generic? If not, ask why. And if the answer isn’t one of the three BNF exceptions-change it.
Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same quality, strength, purity, and potency standards as brand-name drugs. Regulatory bodies like the FDA, EMA, and MHRA require identical active ingredients and bioequivalence testing. The only differences are in inactive ingredients (like fillers or coatings), which rarely affect safety or effectiveness.
Can I switch a patient from a brand to a generic without warning?
For most drugs, yes. But for narrow therapeutic index drugs (like warfarin, levothyroxine, or phenytoin), or modified-release formulations, you should not switch without monitoring. Always check the BNF’s exceptions list. When in doubt, stay with the brand-or consult a pharmacist.
Why are biologics always prescribed by brand name?
Biologics are complex proteins made from living cells. Even small changes in manufacturing can affect how the immune system reacts. Switching between a brand and a biosimilar can increase the risk of immune responses or reduced effectiveness. That’s why the MHRA and FDA require brand-name prescribing for all biologics-no automatic substitution allowed.
Do generic drugs cause more side effects?
No. Large-scale studies show no difference in side effect rates between generics and brands. When patients report side effects after switching, it’s often the nocebo effect-belief that generics are inferior. Clear communication from the prescriber reduces these reports by more than half.
What should I do if a patient refuses a generic?
Listen. Don’t argue. Ask why they’re concerned. Then explain: same active ingredient, same testing, same effectiveness, lower cost. If they still refuse, document it. You can prescribe the brand-but make sure it’s not because of misinformation. Offer to recheck in a month. Many patients change their minds after seeing the savings.
Is generic prescribing mandatory in the UK?
It’s not legally mandatory, but it’s the clear professional standard. NHS England expects 90%+ of prescriptions to be generic. Prescribing brands without clinical justification can trigger audit, feedback, or even financial review by your local CCG. It’s not about punishment-it’s about accountability.
How do I know which drugs have generic alternatives?
Use the British National Formulary (BNF) or your e-prescribing system’s built-in generic check. Most systems flag when a brand has a generic equivalent. If you’re unsure, ask your pharmacist. Over 90% of commonly prescribed drugs have a generic version available.


Gregory Parschauer
January 13, 2026 AT 20:10Let me just say this: if you're still prescribing brand-name statins in 2025, you're not a clinician-you're a corporate shill for Big Pharma. The data is irrefutable. Atorvastatin is atorvastatin. Lipitor is a marketing gimmick wrapped in a white coat. I've seen patients cry because they couldn't afford their 'brand' meds-then they switched to generic and got their life back. This isn't cost-cutting. It's moral obligation.
jefferson fernandes
January 15, 2026 AT 09:11Exactly. And let’s not forget: the FDA, EMA, and WHO all mandate bioequivalence testing for generics-meaning the active ingredient must be identical within 90–110% of the brand’s concentration. That’s not ‘close enough’-that’s scientifically identical. The only differences are in fillers, dyes, or coatings-ingredients that rarely, if ever, affect therapeutic outcomes. So why do we still let patients believe otherwise? Because we don’t educate them properly. We need to change the script.
sam abas
January 16, 2026 AT 03:47Okay but… what about the 2% of cases where it actually matters? Like levothyroxine? I’ve had patients go into atrial fibrillation after switching generics because the bioavailability shifted slightly. Not because the drug was bad-because the manufacturing process changed. And yeah, I know the BNF says ‘monitor’-but monitoring is a pain in the ass. And who’s gonna pay for the extra labs? The patient? The clinic? No one. So we just… keep prescribing the brand. Because it’s easier. And honestly? I’m tired of being guilt-tripped for doing what’s practical, not just what’s ‘ideal’.
Angel Tiestos lopez
January 16, 2026 AT 18:12Bro. 🤔 Generics = same active ingredient. Brand = same active ingredient + fancy packaging + ads on TV. Why are we still acting like this is a mystery? It’s like buying the same coffee but paying $10 more because it’s in a branded cup. The beans are the same. The roast is the same. The caffeine? Identical. We just need to stop letting marketing trick us into thinking price = power. 💪💊
Robin Williams
January 16, 2026 AT 18:58Y’all are overcomplicating this. It’s simple: if you can save someone $12 a month on their meds, and they’re not going to die because of it-DO IT. You’re not just prescribing a pill-you’re prescribing dignity. A roof. Food. A chance. This isn’t about pharmacology. It’s about humanity. And if you’re hesitating? Ask yourself: would I want my mom on Lipitor because it’s ‘better’? Or would I want her to have her life back on $2.50 a month? 🙏
Anny Kaettano
January 17, 2026 AT 19:34I’ve been in primary care for 14 years. I’ve seen the nocebo effect firsthand. Patients come in saying, ‘This generic made me dizzy’-but when I check their logs, their labs are perfect. Their BP? Stable. Their HbA1c? Better. They’re just scared. So I don’t say ‘it’s just a generic.’ I say, ‘This is the exact same medicine your body’s been using, just without the brand logo.’ And then? They breathe easier. The trust rebuilds. And the adherence spikes. It’s not magic. It’s communication.
Kimberly Mitchell
January 18, 2026 AT 13:06Let’s be real. The NHS saving £1.3 billion? That’s not a win-it’s a band-aid on a hemorrhage. We’re pushing generics because the system is broke, not because it’s better care. And don’t get me started on the pressure to hit 92% targets. It’s bureaucratic coercion disguised as clinical excellence. And the real cost? Patient anxiety. Lost trust. And the fact that we’ve turned prescribing into a KPI instead of a clinical decision. This isn’t progress. It’s performance theater.
Angel Molano
January 20, 2026 AT 05:34Stop. Just stop. If you’re prescribing brand-name metformin, you’re committing malpractice. End of story. No exceptions. No excuses. Your patients aren’t your customers. They’re your responsibility. Get with the program.
Vinaypriy Wane
January 21, 2026 AT 07:53I come from a country where generics are the only option-and I’ve never seen a single patient suffer because of it. In fact, adherence is higher. Why? Because they can afford it. We don’t have the luxury of brand names. But we have the wisdom of science. The WHO says it’s safe. The FDA says it’s safe. The patients? They live. They thrive. So why are we in the West still acting like generics are a compromise? It’s not a compromise. It’s common sense.
Diana Campos Ortiz
January 21, 2026 AT 17:01One of my patients switched from brand-name sertraline to generic and said, ‘I feel like I’m waking up from a fog.’ She’d been on it for 8 years. Never realized her mood was off because the brand was inconsistent. Generics aren’t ‘weaker’-sometimes they’re just more consistent. And honestly? The placebo effect works both ways. If you believe it works, it does. So why not believe in the science?
Jesse Ibarra
January 23, 2026 AT 09:35Oh wow. Another sanctimonious lecture from the medical elite. Let me guess-you also think people should eat kale and meditate to cure hypertension? This isn’t about ‘professional responsibility.’ It’s about control. You want to dictate what patients get. You want to erase choice. You want to turn healthcare into a spreadsheet. And you call it ‘evidence-based’? Please. Real medicine isn’t about hitting targets. It’s about listening. And some patients? They need the brand. And that’s okay.
laura Drever
January 24, 2026 AT 01:20Generic prescribing? Sure. But the real issue? The fact that 40% of patients don’t even know what INN stands for. And the system doesn’t care. We’re pushing this without patient education. We’re automating it. We’re not teaching. We’re just prescribing. And then we wonder why people distrust medicine. 🙄
Randall Little
January 25, 2026 AT 22:37So let me get this straight: you’re telling me that a $30 brand-name drug and a $2.50 generic are functionally identical… but we still have 15 different names for the same molecule? Then why are we still using brand names at all? Isn’t that like calling every pair of jeans ‘Levi’s’ even when they’re not? The system is broken. Not the generics. The branding. The language. The confusion. Fix the system, not the prescription.
Lethabo Phalafala
January 26, 2026 AT 11:22I’m from Johannesburg. We’ve been on generics since the 90s because we had no choice. We lost 12,000 people to HIV because they couldn’t afford the brand. Then generics came. And suddenly, millions lived. Now you’re acting like this is some revolutionary idea? This isn’t innovation. This is survival. And if you’re still arguing about it? You’ve never had to choose between rent and your child’s meds.