Many people take multiple medications every day - some prescribed, some bought over the counter, some picked up because "it can’t hurt." But what if some of those pills aren’t helping anymore? What if they’re costing you hundreds a year - and even making you sicker?
Deprescribing isn’t about quitting meds cold turkey. It’s about working with your doctor to safely stop the ones that don’t belong anymore. And it’s one of the most effective ways to cut your drug costs without sacrificing your health.
Why You Might Be Taking Pills You Don’t Need
Most people don’t start out with 10 prescriptions. It happens slowly. A pill for acid reflux leads to another for the side effect of that pill. A sleep aid gets added after a hospital stay. A vitamin gets recommended by a friend. Over time, your medicine cabinet becomes a cluttered shelf of bottles you forgot why you started.
According to the CDC, 44% of adults over 65 take five or more medications. That’s called polypharmacy - and it’s not harmless. Each extra pill adds risk: dizziness, confusion, falls, kidney stress, even memory loss. And it adds up financially. A single $50-a-month pill you no longer need costs $600 a year. Three of them? $1,800. That’s not just waste - it’s a financial burden.
Studies show that up to 37% of hospitalizations in older adults are caused by medication problems - and most of them are preventable. The Lown Institute calls medication overload America’s other drug problem. And the fix? Deprescribing.
What Deprescribing Really Means
Deprescribing is the planned, gradual stopping of medications that are no longer helping - or that do more harm than good. It’s not quitting. It’s rethinking.
For example, a 75-year-old with mild high blood pressure might have been on a beta-blocker for 15 years. But if their blood pressure is now stable and they’ve lost weight, improved their diet, and exercise regularly, that pill may no longer be necessary. Or someone on a proton pump inhibitor (PPI) for heartburn after a short illness - those drugs are meant for short-term use, yet many stay on them for years. Stopping them safely can cut costs by $400 a year and lower the risk of pneumonia.
Deprescribing follows clear guidelines. The American Academy of Family Physicians recommends a four-step process:
- Bring all your meds - every pill, patch, supplement, and OTC drug - to your appointment. This is called a "brown bag review." On average, patients bring 2.3 unnecessary medications to these reviews.
- Review each one using tools like the Beers Criteria, which lists 53 medications that are risky for older adults.
- Decide together which ones to stop, how fast, and what to watch for.
- Check back - follow up in 4 to 12 weeks. Some meds need to be tapered slowly to avoid rebound effects.
It’s not magic. It’s methodical. And it works. Kaiser Permanente’s deprescribing program reduced medication costs by $1.2 million in one year and cut adverse drug events by 28%.
How to Prepare for the Conversation
Doctors are busy. Appointments average 15 minutes. If you walk in without a plan, you’ll likely leave with the same script.
Here’s how to make this conversation count:
- Make a list - write down every medication, including doses and why you take it. Include vitamins, herbal supplements, and pain relievers like ibuprofen or melatonin.
- Note the cost - write down what each one costs per month. You’ll be surprised how quickly the numbers add up.
- Ask these five questions:
- Why am I taking this?
- What’s it supposed to do for me?
- Could it cause dizziness, falls, or memory issues?
- Can I stop it - or lower the dose?
- Who should I call if I feel different after stopping?
- Bring your pharmacy receipt - if you use a mail-order pharmacy, print your last 3 months of charges. That’s real data your doctor can use.
Doctors who get this info say it makes deprescribing discussions 68% more productive. You’re not challenging them - you’re helping them do their job better.
What to Expect When You Start Stopping
Some people worry: "What if I feel worse?" That’s valid. But the risk of staying on something you don’t need is often higher than stopping it safely.
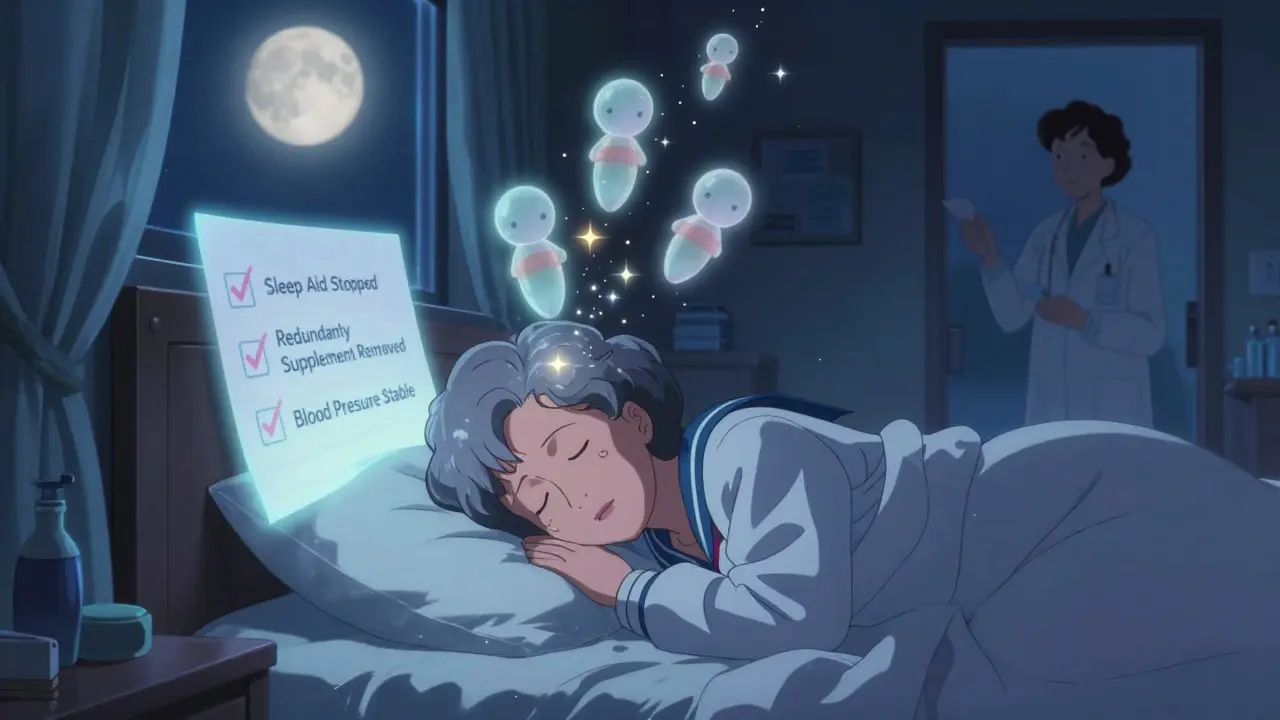
Good deprescribing means going slow. You won’t stop five pills at once. Usually, one at a time. For example:
- A sleep aid like diphenhydramine (Benadryl) might be stopped over 2 weeks - you might feel a little restless at first, but that passes.
- An antihypertensive might be cut in half for 2 weeks, then stopped. Blood pressure is checked weekly.
- A statin for cholesterol might be paused if you’re over 75 with no heart disease history - studies show no increased risk of heart attack when stopped appropriately.
Withdrawal symptoms are rare if done right. But if you stop something too fast - like an antidepressant or blood pressure pill - you can get rebound effects. That’s why doctor guidance matters.
Real patient stories show the savings: A 72-year-old woman in Ohio stopped three unnecessary pills - a $120/month sleep aid and two supplements her cardiologist said were redundant. She saved $840 a year. A Reddit user in Washington state cut a $90/month vitamin D supplement and a $75/month herbal remedy after blood tests showed normal levels. Annual savings: $1,980.
Where to Get Help Beyond Your Doctor
You don’t have to do this alone. Your pharmacist is a hidden ally.
Under Medicare Part D, most community pharmacies offer Medication Therapy Management (MTM) - free of charge. These are 30-minute sessions with a pharmacist who reviews your whole regimen. They spot duplicates, check for interactions, and suggest cheaper alternatives. One 2022 study found pharmacists identified $1,200 in annual savings per patient on average.
Some health systems, like Kaiser Permanente and VA hospitals, have dedicated deprescribing teams. Ask your doctor if your clinic offers one.
And don’t ignore tools like MedStopper - an AI system used by over 120 hospitals to flag unnecessary meds. It’s not perfect, but it’s getting better. Your doctor might not use it, but you can ask: "Is there a tool that helps check if my meds are still needed?"
When Deprescribing Might Not Be Right
Not every pill can or should be stopped. Some meds serve multiple purposes. For example:
- A blood pressure pill might also help prevent migraines.
- An antidepressant might be used for nerve pain.
- A low-dose aspirin might be prescribed for heart protection, not just pain.
That’s why you need a doctor’s input. Never stop a medication on your own - especially blood thinners, seizure drugs, or steroids. The National Council on Aging found that 18% of people who tried self-deprescribing ended up in the ER with avoidable problems - costing an average of $1,200 in extra care.
Deprescribing only works when it’s planned, monitored, and personalized.
The Big Picture: Why This Matters Now
Prescription drug prices have risen 60% since 2014. For seniors on fixed incomes, meds now eat up 18.3% of their monthly income. The Inflation Reduction Act capped insulin at $35/month - a huge win - but most other drugs are still unaffordable.
Deprescribing is one of the few strategies that cuts costs and improves safety. The US Deprescribing Research Network estimates that if everyone who needed to stop unnecessary meds did so safely, Medicare could save $2.8 billion a year.
And it’s getting easier. Since 2023, Medicare Advantage plans are being scored on medication safety. Hospitals and clinics now get paid more for helping patients reduce risky prescriptions. That means more doctors are being trained - and more programs are being launched.
It’s not about cutting corners. It’s about cutting clutter. Your body isn’t a warehouse for pills. It’s a system that works best when it’s not overloaded.
Next Steps: What to Do Today
You don’t need to wait for your next appointment. Start now:
- Grab all your medications - bottles, boxes, supplements, patches.
- Write down each one: name, dose, why you take it, and monthly cost.
- Call your pharmacy and ask: "Can I schedule a free Medication Therapy Management session?"
- Write down your top 3 questions to ask your doctor.
- Bring your list to your next visit - and don’t leave without a plan.
Deprescribing isn’t a one-time event. It’s a habit. Review your meds every year. Ask the same five questions. If something doesn’t make sense anymore - say so.
Your wallet - and your body - will thank you.
Is deprescribing safe?
Yes - when done correctly under medical supervision. Stopping medications too quickly can cause rebound effects, like higher blood pressure or rebound insomnia. But a structured plan - tapering slowly, monitoring symptoms, and checking in regularly - makes it safe. Studies show that when done properly, deprescribing reduces adverse events by up to 28%.
Can I stop taking my meds on my own?
No. Never stop a prescribed medication without talking to your doctor. Some drugs - like blood thinners, antidepressants, seizure meds, or steroids - can cause serious withdrawal effects if stopped suddenly. Even "harmless" supplements can interact with prescriptions. The National Council on Aging found that 18% of people who tried self-deprescribing ended up needing emergency care.
What if my doctor says no to deprescribing?
Ask why. If they say "it’s just in case," push back. Ask for evidence: "Is there a study showing this still helps me?" If they’re unsure, ask for a referral to a geriatrician or a pharmacist who specializes in medication reviews. You have the right to understand every medication you take. If your doctor dismisses your concerns, consider finding a provider who supports shared decision-making.
How long does it take to see savings from deprescribing?
Almost immediately. If you stop a $75/month pill, you save $75 the next month. But some savings come later - like avoiding a fall or hospitalization. A single medication-related hospital stay costs an average of $15,700. That’s why the long-term savings are often bigger than the monthly drug savings.
Does insurance cover deprescribing services?
Yes - under Medicare Part D, most pharmacies offer free Medication Therapy Management (MTM) sessions. These are 30-minute appointments with a pharmacist who reviews your whole regimen for safety and cost. Many Medicare Advantage plans also cover comprehensive medication reviews. Ask your pharmacist or insurance provider: "Do I qualify for a free medication review?"


Lauren Warner
January 12, 2026 AT 00:42Deprescribing is the most underutilized tool in modern medicine. I’ve seen patients on 12 meds who didn’t need half of them. One 80-year-old was taking a statin, a PPI, a sleep aid, two supplements, and an antihistamine-all for conditions that had resolved years ago. We tapered one by one over three months. His cognition improved, his falls stopped, and his monthly bill dropped from $412 to $87. No drama. Just common sense.
Doctors don’t get paid to deprescribe. Pharmacies profit from continuity. It’s a system designed to keep you medicated, not healthy.
Craig Wright
January 12, 2026 AT 23:19It is imperative to acknowledge that the structural incentives within the American healthcare system are fundamentally misaligned with patient welfare. The pharmaceutical-industrial complex thrives on perpetual pharmacotherapy, and deprescribing represents a direct challenge to its economic model. The fact that Medicare now incentivizes medication reviews is a modest corrective, but insufficient without broader regulatory intervention. One must question the ethics of a system where financial gain supersedes clinical necessity.
Lelia Battle
January 13, 2026 AT 15:15I’ve been thinking about this for years-not just as a patient, but as someone who’s watched my mother’s medication list grow from three to twelve over a decade. It’s not just about cost. It’s about identity. We start to believe the pills are who we are. ‘I’m the person who takes the blue pill for sleep, the red one for blood pressure, the green one for memory.’ But what if we’re just the person who’s been told to take them?
Deprescribing isn’t just medical. It’s existential. It asks: Who are you without the bottles?
Darryl Perry
January 15, 2026 AT 07:13Stop taking supplements. Done.
Jose Mecanico
January 16, 2026 AT 13:13This is spot on. My dad went through this last year. He was on a PPI for five years after a short bout of heartburn. Turned out he never needed it. Stopped it slowly, no issues. Saved $500 a year and stopped feeling bloated all the time. Took him six months to admit he didn’t need it. Doctors don’t always push back, but they should.
George Bridges
January 16, 2026 AT 20:00I appreciate how this post breaks down the steps. My mom’s pharmacist did a free MTM session last month and found three duplicate meds she didn’t even know she was taking. One was an old blood thinner that was never discontinued after her stent. We almost missed it. Pharmacists are unsung heroes here.
gary ysturiz
January 17, 2026 AT 07:28You don’t need to be sick to be overmedicated. That’s the real truth here. We treat symptoms like enemies instead of signals. Sometimes the body just needs space to heal, not more pills. I’ve cut my own meds twice now-first a sleep aid, then a vitamin D. Felt better both times. No magic. Just listening.
Start small. One pill at a time. Talk to your doc. You’ve got nothing to lose but the clutter.
Jessica Bnouzalim
January 18, 2026 AT 11:32OMG YES. I stopped my 1000mg vitamin C and my 'energy' gummies last year and my anxiety actually got better?? Like, who knew? I thought I was being healthy, but turns out I was just throwing money at a bottle labeled 'maybe helps'? 🤦♀️ Saved $70/month. Also, my sleep improved. Who knew supplements could mess with your brain?!
Sumit Sharma
January 19, 2026 AT 20:55From a clinical pharmacology perspective, polypharmacy in geriatric populations remains a critical public health concern. The Beers Criteria are evidence-based, yet underutilized due to cognitive load and time constraints in primary care. The 37% hospitalization statistic is corroborated by multiple cohort studies, including the 2021 JAMA Internal Medicine analysis. Pharmacist-led MTM interventions demonstrate a 22–34% reduction in adverse drug events. The cost-benefit ratio is unequivocal. Systemic adoption is not optional-it is imperative.
Katherine Carlock
January 21, 2026 AT 03:53My grandma started this process last year and now she’s the one telling everyone else to do it. She said, 'I used to feel like a pharmacy. Now I feel like me again.' She still takes her blood pressure med and her thyroid pill, but everything else? Gone. And she’s happier. I think we forget that meds aren’t just for the body-they’re for the mind too. Sometimes, letting go of the bottle lets you let go of the fear.
beth cordell
January 22, 2026 AT 01:45❤️ This needs to be on every doctor’s waiting room wall. I took my mom to her first MTM session and the pharmacist cried when he saw her list. 17 meds. She was 78. Now she’s down to 5. She says she can finally walk to the mailbox without feeling like a zombie. Thank you for writing this.
Daniel Pate
January 23, 2026 AT 04:50What’s the long-term data on deprescribing for people under 65? Most studies focus on seniors, but I’ve seen young adults on SSRIs for anxiety they got after a breakup-five years later. Are we just medicalizing normal human stress? Is deprescribing just a fancy word for 'stop being lazy and deal with your life'? Or is there real science behind tapering in younger populations?
Amanda Eichstaedt
January 24, 2026 AT 11:36I’ve been doing this for years. Not just with meds, but with everything. We’re taught to add, never to remove. More pills, more apps, more subscriptions, more stuff. But the body doesn’t need more. It needs clarity. I stopped taking my daily multivitamin after a blood test showed I was fine. I stopped my nightly melatonin after I fixed my sleep schedule. I stopped my expensive protein powder after I realized I was getting enough from food.
Deprescribing isn’t just about pills. It’s about learning what you actually need. And letting go of the rest.
It’s not a trend. It’s a return to sanity.