Every year, more than 120,000 people in the U.S. die from lung cancer. Most of them were never tested until it was too late. But there’s a simple scan that can catch it early-when it’s easiest to treat. It’s called low-dose CT for lung screening. And if you’re in a high-risk group, it could save your life.
Who Should Get a Low-Dose CT Scan for Lung Cancer?
You don’t need this scan if you’ve never smoked. But if you have a history of smoking, the rules are clear. The U.S. Preventive Services Task Force says you should be screened annually if you’re between 50 and 80 years old, have smoked at least 20 pack-years, and either still smoke or quit within the last 15 years.
What’s a pack-year? It’s simple: one pack a day for one year equals one pack-year. So if you smoked a pack a day for 20 years, that’s 20 pack-years. Or two packs a day for 10 years. Or half a pack a day for 40 years. It adds up.
Some guidelines, like those from the American Cancer Society and the National Comprehensive Cancer Network, go even further. They say you might still benefit even if you quit more than 15 years ago-especially if you have other risk factors like a family history of lung cancer, exposure to asbestos or radon, or a history of lung disease like COPD or pulmonary fibrosis.
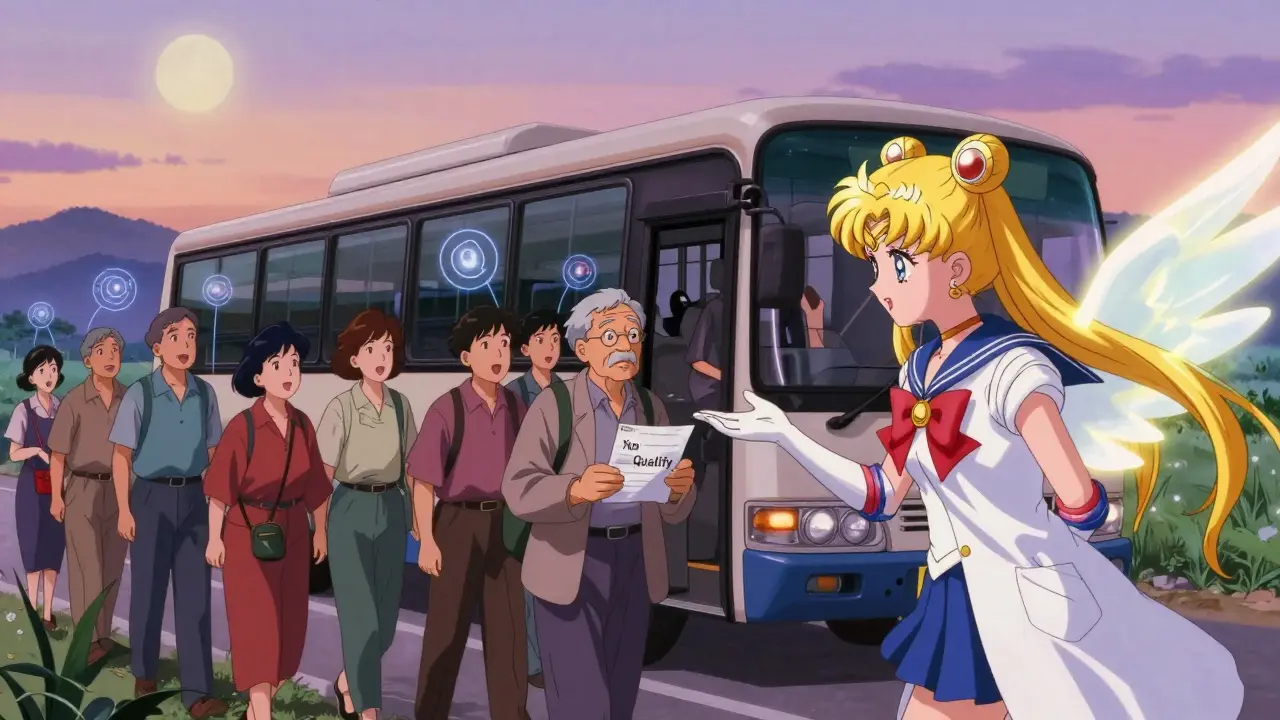
But here’s the catch: only about 1 in 5 eligible people actually get screened. Why? Many don’t know they qualify. Others are scared of false alarms. Some can’t get to a clinic-especially in rural areas where the nearest screening center might be 30 miles away.
What Happens During the Scan?
The scan itself takes less than 10 seconds. You lie on a table, raise your arms, and hold your breath while the machine spins around you. No needles. No fasting. No contrast dye. Just a quick, painless image of your lungs.
What makes it “low-dose”? Standard CT scans use about 7-10 mSv of radiation. A low-dose CT uses less than 1.5 mSv-roughly one-tenth of that. That’s about the same radiation you’d get from natural background sources over six months. The risk from this level of radiation is extremely low. In fact, for every 1,000 people screened, you might prevent 15 lung cancer deaths while causing maybe one extra cancer from radiation. The math is clear: you’re trading a tiny risk for a huge benefit.
Modern machines use advanced software to cut dose even further. Some now deliver scans at just 0.8 mSv. And the images are reconstructed with algorithms that sharpen details without adding noise. This helps radiologists spot tiny nodules-sometimes as small as 4 millimeters-that would be invisible on a regular X-ray.
What Do the Results Mean?
Most scans-about 75%-come back normal. No nodules. No worries. You’ll be told to come back in a year.
But about 1 in 4 scans show something unusual. That doesn’t mean cancer. In fact, more than 96% of all positive findings turn out to be harmless. They could be scars from old infections, enlarged lymph nodes, or benign growths.
Still, any nodule larger than 4 mm triggers follow-up. The next step? Usually another low-dose CT in 3 to 6 months. If it grows, you might need a PET scan or biopsy. If it stays the same or shrinks, you’re likely fine and can return to annual screening.
The biggest challenge isn’t finding cancer-it’s handling the anxiety that comes with a positive result. A 2023 survey found that 42% of people felt intense worry during the wait for follow-up tests. One woman from Ohio, Mary Johnson, said her scan found a 6mm nodule. It turned out to be Stage 1 adenocarcinoma. She had surgery and is now cancer-free. Another man, James Wilson from Texas, spent three months in stress and paid $450 in out-of-pocket costs before his nodule was ruled benign.
That’s why shared decision-making matters. Before your first scan, your provider should sit down with you for 25-30 minutes. They’ll explain the risks, the benefits, and what happens if something shows up. This isn’t just paperwork-it’s part of the process. Medicare requires it. Accredited centers must document it.
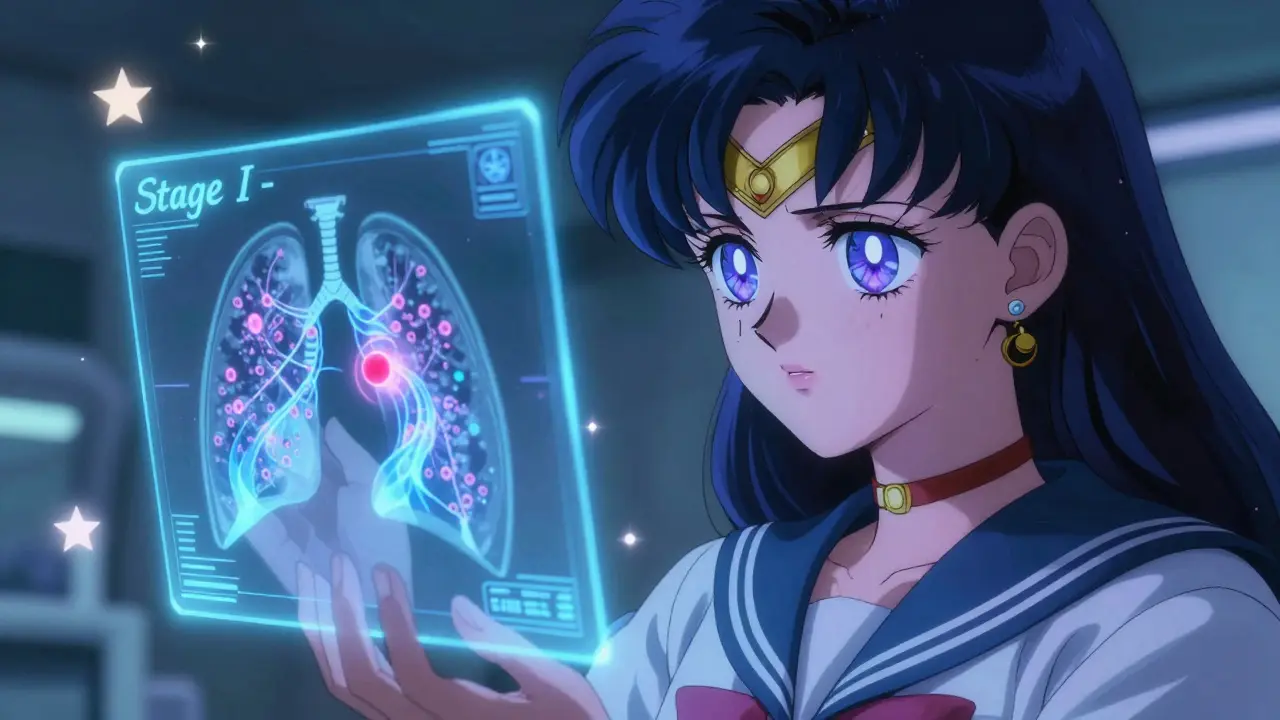
What Happens If Cancer Is Found?
If a scan finds cancer, the good news is it’s usually caught early. In the National Lung Screening Trial, 71% of cancers found by LDCT were Stage I-meaning they hadn’t spread beyond the lung. That’s more than double the rate seen with chest X-rays.
Stage I lung cancer is often curable. Most patients get surgery-usually a minimally invasive procedure called VATS (video-assisted thoracic surgery). Recovery is faster: hospital stays dropped from over five days to just over three. Complication rates are under 1% in high-volume centers.
Some patients may need radiation or targeted therapy, depending on the cancer type. But early detection changes everything. One study showed that people who caught their cancer through screening lived an average of 10 years longer than those diagnosed after symptoms appeared.
Why Isn’t Everyone Getting Screened?
Even though the evidence is solid and the cost is covered by Medicare and most private insurers, uptake is still low. Only 23% of eligible Americans get screened. That’s up from 4% in 2016, but it’s nowhere near where it should be.
Barriers are real. In rural areas, distance is the biggest problem. The average person lives 32 miles from a screening center. Transportation, lack of time, and distrust in the system keep people away. Black Americans are 15% more likely to get lung cancer than White Americans-but they’re screened at 28% lower rates.
States that expanded Medicaid have screening rates nearly 40% higher than those that didn’t. That’s not a coincidence. Access matters.
Another issue? Many doctors don’t bring it up. If your primary care provider doesn’t ask about your smoking history or mention screening, you won’t know to ask. That’s changing slowly. More clinics now use electronic alerts to remind providers when a patient qualifies.
What’s Next for Lung Screening?
Experts are working on smarter ways to find who needs screening most. Right now, eligibility is based on age and smoking history. But that’s like using a hammer to fix a watch.
New risk models-like the LYFS-CT model-are being tested. They look at age, smoking, family history, COPD, and even blood markers. One study showed these models could improve screening efficiency by 27%, meaning fewer people get scanned unnecessarily, and more high-risk people are caught early.
AI is helping too. Software like LungPoint® can analyze scans faster and with 97% accuracy. Radiologists can read scans in half the time, reducing backlogs and errors.
And the rules might change soon. In January 2024, Medicare announced it’s reviewing whether to remove the 15-year quit limit. If they do, millions more people-especially those who quit decades ago-could qualify. One analysis says that change alone could prevent 12,000 more deaths each year.
Bottom Line: Don’t Wait for Symptoms
Lung cancer doesn’t cause symptoms until it’s advanced. By then, it’s often too late. Low-dose CT screening is the only proven way to catch it early in people who’ve smoked.
If you’re between 50 and 80, have smoked 20 pack-years or more, and either still smoke or quit within the last 15 years-you qualify. Talk to your doctor. Ask for the scan. It’s free with most insurance. It takes less than a minute. And it might give you another decade.
Don’t let fear of false positives stop you. Most of them are nothing. And if something is found, catching it early gives you the best shot at living a full life.


Lydia H.
January 19, 2026 AT 21:42My uncle got screened last year after his doctor finally brought it up. Turned out to be a 5mm nodule. Three months later, it was gone. No surgery, no chemo. Just a scan and a sigh of relief. I wish more people knew this was an option.
Josh Kenna
January 20, 2026 AT 10:59im so tired of people being scared of radiation from scans. like bro you’re literally risking death by not getting checked. the amount of radiation from one of these is less than you get from a cross-country flight. and if you smoke? you’re already poisoning yourself daily. this is the easiest life hack ever.
Jacob Hill
January 20, 2026 AT 11:19I appreciate the thorough breakdown, but I think we’re underestimating the psychological toll of false positives. I know someone who waited six weeks for a follow-up scan-she couldn’t sleep, lost 12 pounds, and quit her job out of fear. The medical system treats this like a checklist item, but it’s not. The anxiety is real, and it’s not accounted for in the stats.
Lewis Yeaple
January 22, 2026 AT 03:38It is imperative to note that the United States Preventive Services Task Force (USPSTF) guidelines are evidence-based and widely accepted by the American College of Radiology, the American Lung Association, and the National Cancer Institute. Any deviation from these criteria without robust clinical justification constitutes a deviation from standard of care.
sujit paul
January 23, 2026 AT 23:18Let me ask you this: who really benefits from these scans? The hospitals? The radiology equipment companies? The pharmaceutical giants who profit from chemo and surgery? The government? I’ve seen too many people get scanned, get scared, get biopsied, and end up with a bill they can’t pay-while the system smiles and says, "We saved a life." But at what cost? The truth is buried under data.
Christi Steinbeck
January 25, 2026 AT 06:39Stop waiting for your doctor to bring it up. Go to your clinic. Say, "I’m 55, smoked for 22 years, I want my low-dose CT." They can’t say no. It’s covered. It’s fast. It’s free. If you’re eligible, you owe it to your family to get it done. No excuses.
Tracy Howard
January 25, 2026 AT 15:16It’s hilarious how Americans treat this like some revolutionary breakthrough. In Canada, we’ve had lung screening programs since 2018 in Ontario. We don’t need to beg our doctors-we just get it. And no, we don’t have the same cancer rates. Maybe if you stopped blaming the system and started taking responsibility, you’d live longer.
Jake Rudin
January 27, 2026 AT 01:56What’s fascinating is how the 15-year quit cutoff is arbitrary. It’s based on population-level risk curves, not biology. Someone who quit 20 years ago but had COPD and lived near a coal plant? Their risk profile is identical to someone who quit 10 years ago. The system needs to move beyond binary checkboxes and into dynamic risk modeling-like the LYFS-CT model mentioned. It’s not just better-it’s inevitable.
Astha Jain
January 28, 2026 AT 03:58why do u think the gov wants u to get scanned? its not about health... its about control. once u start getting scanned, they can track ur lungs, ur habits, ur data... next thing u know, ur insurance raises ur rates because u "have a nodule" even if its benign. this is surveillance disguised as care.
Phil Hillson
January 29, 2026 AT 18:26So let me get this straight… we’re telling people to get a scan that might give them cancer from radiation, then making them pay hundreds for follow-ups that usually turn out to be nothing, and calling it a win? I mean… I guess if your goal is to traumatize smokers and line the pockets of radiologists, then yeah, this is genius. The real win? Not smoking in the first place.
Jackson Doughart
January 30, 2026 AT 16:23Thank you for writing this with such clarity. I’ve worked in primary care for 18 years, and I’ve seen too many patients who didn’t know they qualified. I now have a printed one-pager I hand out to every smoker over 50. It’s not about fear-it’s about empowerment. If you’re eligible, you deserve to know. And if you’re not sure? Ask. It’s that simple.