Every year, thousands of people end up in emergency rooms or die from drug combinations they thought were safe. It’s not always illegal drugs. Often, it’s prescription pills mixed with alcohol, or over-the-counter meds taken with antidepressants. The truth? Some combinations don’t just increase side effects-they multiply danger. And many people don’t realize they’re at risk until it’s too late.
Why Some Drug Mixes Are Deadly
Not all drug interactions are the same. Some cause mild nausea or drowsiness. Others shut down your breathing, stop your heart, or destroy your liver. The most dangerous combinations work by amplifying effects you can’t feel until it’s too late. Think of it like turning up two volume knobs at once-each one is loud on its own, but together, they blast your system past its limit. The biggest killers fall into three categories: central nervous system depressants, stimulant-depressant pairs, and metabolically toxic mixes. Each one has a different mechanism, but all lead to the same outcome: organ failure, overdose, or sudden death.Opioids + Alcohol: A Silent Killer
Opioids like oxycodone, hydrocodone, and fentanyl are powerful painkillers. Alcohol is a depressant. Together, they slow your breathing to a dangerous crawl. Research shows this combo increases the risk of respiratory failure by 4.5 times compared to either substance alone. People often don’t think of it as risky. They take their prescribed painkiller after a long day and have a glass of wine to unwind. But even one or two drinks can push your body over the edge. A Reddit user shared how they had two drinks after dental surgery and went into respiratory arrest-only saved by naloxone. That’s not rare. In 2020, 30.1% of opioid overdose deaths also involved alcohol. The body doesn’t handle this well. Dizziness, confusion, extreme drowsiness, and unconsciousness can come on fast. And because opioids dull pain and alcohol dulls awareness, you might not realize how close you are to stopping breathing until it’s too late.Benzodiazepines + Opioids: The Most Common Deadly Mix
Benzodiazepines-like Xanax, Valium, and Ativan-are prescribed for anxiety, insomnia, or muscle spasms. They work on the same brain receptors as opioids. When combined, they don’t just add up-they multiply. The CDC found that in over 30% of fatal opioid overdoses, benzodiazepines were also present. That’s not a coincidence. This combo causes profound sedation, muscle weakness, and dangerously low breathing rates. Some patients drop below 10 breaths per minute. At that point, your brain doesn’t get enough oxygen. Brain damage follows quickly. Death can happen within minutes. Even worse, many people don’t realize they’re taking both. A doctor prescribes Xanax for anxiety, and later, painkillers for a back injury. No one connects the dots. That’s why Medicare Part D now flags these combinations automatically. Since 2019, this alert system has cut concurrent prescriptions by 18%.Speedball: Cocaine + Heroin
The so-called “speedball” sounds like a myth, but it’s real-and deadly. Cocaine is a stimulant. Heroin is a depressant. People think they balance each other out. They don’t. They confuse your body’s warning signals. Cocaine spikes your heart rate and blood pressure. Heroin slows your breathing. Together, your heart is racing while your lungs are shutting down. This puts extreme stress on your cardiovascular system. Studies show this combo increases the risk of heart attack, stroke, and sudden cardiac arrest. And it’s not just heroin. Cocaine mixed with any opioid-fentanyl, morphine, codeine-is just as dangerous. In 2021, nearly half of all cocaine overdoses in the U.S. involved an opioid. Celebrities like River Phoenix and Chris Farley died from this mix. But most victims aren’t famous. They’re everyday people who didn’t know what they were taking.
Alcohol + Cocaine: The Hidden Toxin
When alcohol and cocaine are in your system at the same time, your liver creates a new chemical: cocaethylene. It’s more toxic than either drug alone. It lasts longer. It hits harder. Cocaethylene increases the risk of sudden death by 25% compared to cocaine by itself. It causes severe liver damage, irregular heartbeat, seizures, and heart attacks. Chronic users often develop liver disease without knowing why-because the damage is hidden behind the euphoria. Users report feeling more euphoria and longer highs, which makes them take more. But their body can’t process it. The heart struggles. The liver gets overwhelmed. One study found that 65% of regular users of this combo showed signs of liver toxicity.Antidepressants + Alcohol: A Slow Burn
People often think antidepressants are safe with alcohol. They’re not. Mixing alcohol with SSRIs like sertraline or SNRIs like venlafaxine can lower your tolerance to alcohol, making you pass out faster. With venlafaxine, the risk of fatal alcohol overdose increases by 25%. Duloxetine (Cymbalta) is another offender. When combined with alcohol, liver toxicity risk jumps by 40%. This isn’t about getting drunk. It’s about long-term damage. Your liver doesn’t scream until it’s failing. And then there’s buprenorphine-used to treat opioid addiction. It’s supposed to save lives. But if you drink while on it, you can slip into deep sedation, low blood pressure, and coma. The SA Health Department says: “The more alcohol in your body, the less heroin you need to die.” The same applies to buprenorphine.Stimulants + Stimulants: Overload
Mixing cocaine and methamphetamine sounds like a party trick. It’s not. Both push your heart rate and blood pressure to dangerous levels. You feel wired, alert, unstoppable. But your body is running on fumes. This combo increases the risk of psychosis by 35%. Anxiety and panic attacks affect 60-70% of users. Seizures are common. Heart attacks happen without warning. There’s no safety net. Your nervous system is on fire. Even over-the-counter stimulants like pseudoephedrine (in cold meds) can be dangerous if mixed with ADHD meds like Adderall. The result? High blood pressure, chest pain, and stroke risk.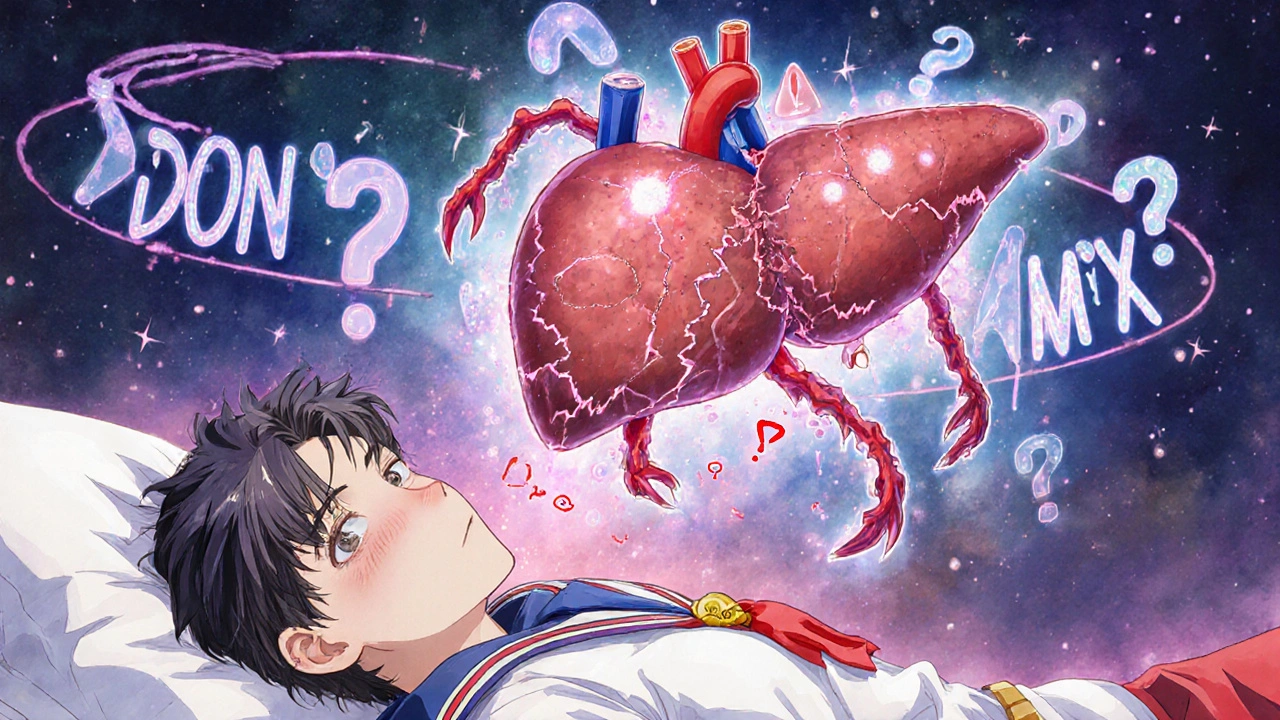
What You Can Do
The good news? Most of these deaths are preventable.- If you’re on opioids, benzodiazepines, or buprenorphine, avoid alcohol completely. Even one drink can be risky.
- Always tell your doctor or pharmacist about every medication, supplement, and recreational drug you use-including CBD, marijuana, or herbal remedies.
- Don’t assume “prescription” means safe. Many dangerous interactions happen because of legal drugs.
- Use free online tools like WebMD’s Drug Interaction Checker or Medscape’s tool. They’re not perfect, but they catch the big red flags.
- If you use street drugs, assume everything is laced with fentanyl. The DEA says 6 out of 10 fake pills contain a lethal dose.
- Carry naloxone if you or someone you know uses opioids. It can reverse an overdose in minutes.
What’s Changing
Hospitals and pharmacies are waking up. Electronic health records now flag dangerous combinations before prescriptions are filled. Poison control centers are seeing a 27% increase in calls about polysubstance use since 2023’s public awareness campaign. By 2025, AI tools will automatically scan your meds and warn your doctor if you’re at risk. That’s progress. But technology won’t save you if you don’t ask the questions.Final Reality Check
You might think, “I’ve done this before and been fine.” So have thousands of others. But one time is all it takes. These combinations don’t care about your experience, your tolerance, or your intentions. They only care about chemistry. Your body doesn’t have a reset button. Once your breathing stops or your liver fails, there’s no undo. The safest choice isn’t moderation-it’s avoidance. If a combination is flagged as dangerous, don’t test it. Don’t rationalize it. Walk away. Your life isn’t worth the risk.Can mixing prescription drugs with alcohol really be deadly?
Yes. Mixing alcohol with opioids, benzodiazepines, or certain antidepressants can slow your breathing to dangerous levels, cause liver failure, or trigger sudden cardiac arrest. Even one drink can increase overdose risk by 20-300%, depending on the drug. The effects are not linear-they multiply.
Is it safe to take painkillers and drink occasionally?
No. Opioid painkillers like oxycodone or hydrocodone combined with alcohol-even one standard drink-can cause respiratory depression, unconsciousness, or death. Studies show a 4.5-fold increase in risk. There is no safe level of alcohol with these drugs.
What is cocaethylene and why is it dangerous?
Cocaethylene is a toxic chemical your liver creates when you mix alcohol and cocaine. It lasts longer in your system than cocaine alone and increases the risk of sudden death by 25%. It also causes severe liver damage, heart rhythm problems, and seizures. Many users don’t realize they’re exposed to it until it’s too late.
Why are benzodiazepines and opioids such a deadly mix?
Both drugs suppress the central nervous system. Together, they dramatically reduce breathing rate and depth. In 2020, over 30% of opioid overdose deaths involved benzodiazepines. This combination can cause coma or death within minutes, even at prescribed doses. Many people don’t know they’re taking both, making it especially dangerous.
Can I use a drug interaction checker to stay safe?
Yes, tools like WebMD’s Drug Interaction Checker or Medscape’s tool can flag major risks like opioid-alcohol or benzodiazepine-opioid combinations. They’re not foolproof, but they catch the most lethal interactions. Always use them before mixing medications, supplements, or alcohol. If a tool flags a combo, talk to your pharmacist immediately.
What should I do if I’ve mixed dangerous drugs and feel unwell?
Call emergency services immediately. Don’t wait. Symptoms like slow breathing, confusion, blue lips, unresponsiveness, or chest pain mean your body is failing. If you have naloxone and suspect opioid involvement, administer it while waiting for help. Time is critical-every minute counts.
Are herbal supplements safe to mix with prescription drugs?
No. Many herbal products like St. John’s Wort, kava, or valerian root interact dangerously with antidepressants, blood thinners, and sedatives. St. John’s Wort can reduce the effectiveness of birth control and antidepressants. Kava can cause liver damage when combined with alcohol or acetaminophen. Always disclose all supplements to your doctor.
Why are fentanyl-laced pills so dangerous in combination with other drugs?
Fentanyl is 50-100 times stronger than morphine. The DEA found that 6 out of 10 fake pills contain a lethal dose. When mixed with alcohol, benzodiazepines, or even small amounts of other opioids, the risk of respiratory arrest skyrockets. Users often don’t know they’re taking fentanyl, making accidental overdose extremely common.


Rhiana Grob
November 26, 2025 AT 12:51This is one of the most important posts I've read all year. Seriously. I work in primary care, and I see people mixing meds and alcohol all the time-thinking they’re being ‘responsible’ because they’re not doing drugs. The truth is, we’re all just one bad combo away from tragedy. Thank you for laying this out so clearly.
Everyone: if you’re on anything that affects your CNS, just say no to alcohol. Full stop. No exceptions. Your liver doesn’t care how ‘moderate’ you think you are.
Also, please tell your doctor about every supplement, herb, or CBD tincture you take. St. John’s Wort isn’t harmless-it’s a silent killer with a smiley face label.
Frances Melendez
November 27, 2025 AT 09:03Of course you’re telling people to avoid alcohol. Because obviously, the real problem is that people like to relax. Not that doctors prescribe 12 different drugs to treat the side effects of other drugs. This is capitalism wrapped in a white coat.
‘Don’t mix opioids with alcohol’-sure, but why are we giving people opioids in the first place? Why are we treating chronic pain like a puzzle to solve with pills instead of listening to the person? You’re treating symptoms while the system rots.
And don’t get me started on ‘naloxone’ as a band-aid. It’s not a solution. It’s a PR stunt.
Kaleigh Scroger
November 28, 2025 AT 07:18Just want to add something the article didn’t cover-SSRIs + NSAIDs like ibuprofen. People think it’s fine because both are ‘over-the-counter’ or ‘prescribed.’ But together, they massively increase GI bleeding risk, especially in older adults. I’ve seen three patients in the last year with ulcers from this combo. One nearly died.
Also, if you’re on warfarin, don’t touch turmeric, garlic supplements, or even green tea in large amounts. The interactions are sneaky. Your doctor probably doesn’t ask about supplements because they’re overwhelmed. But you need to volunteer it. Write it down. Bring a list.
And if you’re on gabapentin? Don’t drink. Even one beer. It’ll knock you flat. I learned that the hard way after a dental procedure. Woke up on the floor. No idea how I got there.
Knowledge is power. But you have to actively seek it. Don’t assume safety. Assume risk. Always.
Jonah Thunderbolt
November 28, 2025 AT 12:53OMG. YES. I KNEW THIS WAS A THING. 🤯😭 I had a friend OD on a ‘speedball’ and I thought it was just a myth until I saw her pupils turn into black holes and her lips turn blue. She was 24. She had a job. She had a dog. She thought she was ‘in control.’
And now I’m just… sitting here wondering why no one taught us this in high school. Like, we had sex ed. We had D.A.R.E. But nothing about how your liver turns into a volcano when you mix cocaine and whiskey?
Also, cocaethylene? That’s a word I needed to hear. Now I’m going to scream it at every party I attend. 🙃 #CocaethyleneIsNotAPartyGuest
Allison Turner
November 29, 2025 AT 08:47This post is so basic. Everyone knows this. Why is this even a thing? Like, really? We need an article to tell us not to mix alcohol and painkillers? What are we, 12?
Also, why is everyone acting like they just discovered this? My grandma knew this in the 70s. She told me not to mix my pills with beer. And I listened. Because she was smart.
Stop making this sound like some deep secret. It’s not. It’s just people being dumb.
Gayle Jenkins
December 1, 2025 AT 05:26Thank you for this. I’m a nurse in the ER, and I see this every weekend. People come in after ‘just one drink’ with their oxycodone. Or they took Xanax before a party and drank to ‘chill out.’
Here’s what I want you to know: it’s not about willpower. It’s about chemistry. Your body doesn’t negotiate. It doesn’t care if you’re ‘funny’ or ‘fun’ or ‘just trying to relax.’ It just shuts down.
And if you’re on buprenorphine? Don’t even think about it. I had a patient die last month after one beer. He thought he was ‘clean’ now. He wasn’t.
Carry naloxone. Know the signs. Talk to your pharmacist. You’re not being paranoid-you’re being smart.
reshmi mahi
December 1, 2025 AT 21:11Why are Americans so scared of everything? In India, we mix chai with painkillers, whiskey with antidepressants, and nobody dies. You people overthink everything. Just take your pills and enjoy life.
Also, who even uses WebMD? That’s for people who Google their symptoms and think they have brain cancer. 🤦♀️
Stop scaring people. Life is short. Drink. Take your meds. Live.
laura lauraa
December 3, 2025 AT 17:41Let’s be honest: the real issue here isn’t drug interactions-it’s the collapse of human dignity in the face of pharmaceutical capitalism. We are not individuals; we are data points in a profit-driven algorithm. Your ‘naloxone’ is a corporate PR tool. Your ‘drug interaction checker’ is a liability shield for Big Pharma.
And yet-you still believe in systems. You still trust the ‘doctor.’ You still think ‘awareness’ will save you.
It won’t.
Because the system doesn’t want you to be well. It wants you to be managed.
And if you’re still reading this, you’re already part of the problem.
…I’m sorry. I just needed to say that. I’ve been holding it in for years.
Darrel Smith
December 4, 2025 AT 12:14I’m a veteran. I’ve been on opioids for 12 years. I drink sometimes. I know the risks. But here’s the thing-I’ve been fine. I’ve had whiskey after my pills for years. I’ve never passed out. I’ve never needed naloxone.
So why should I stop? Because some article says so? Because some doctor says so?
My body knows what it can handle. You don’t know my life. You don’t know my pain. You don’t know my discipline.
Don’t shame people for surviving. Not everyone is weak. Not everyone is a statistic.
And if you’re gonna preach, at least admit that you don’t know what’s true for everyone.
Just saying.
marie HUREL
December 6, 2025 AT 00:13My mom took Xanax and drank wine every night. She died of respiratory failure at 68. No one knew it was the combo. She was ‘just relaxing.’
I didn’t know until the coroner’s report.
Now I tell everyone I know: if you’re on a sedative, don’t drink. Not even one glass. Not even one sip. It’s not worth it.
I wish I’d known sooner.
Thank you for posting this. I’m sharing it with everyone.
Elizabeth Choi
December 6, 2025 AT 04:14Interesting. But where’s the data on non-opioid interactions? Like, what about statins + grapefruit? Or metformin + alcohol? Or levothyroxine + calcium supplements? You cherry-picked the flashy ones. The real danger is the quiet ones.
Also, you mentioned ‘herbal remedies’ but didn’t list specific ones that interact with anticoagulants. That’s lazy.
This feels like fearmongering with a side of clickbait.
Alex Hess
December 7, 2025 AT 21:58Wow. Such a profound, deeply researched, and utterly banal piece of content. You’ve managed to restate what every medical student learns in their first semester, wrapped in the emotional packaging of a TED Talk gone wrong.
‘Cocaethylene’? Groundbreaking. ‘Naloxone saves lives’? Revolutionary. ‘Don’t mix alcohol and opioids’? Who knew?
Did you also consider that people might be self-medicating because the healthcare system failed them? That perhaps the real red flag isn’t the drug combo-but the fact that people are desperate enough to risk their lives just to feel normal?
But no. Let’s just blame the users. Always the users.
Classic.
Rebecca Price
December 9, 2025 AT 19:55Thank you for this. I’m a mother of two, and I used to think ‘just one drink’ was harmless with my antidepressants. Then I blacked out during a family dinner. I woke up on the floor. My daughter was crying. My husband was screaming for an ambulance.
Turns out, I had taken sertraline and had two glasses of wine. My liver enzyme levels were through the roof.
I’ve been sober for 11 months now. Not because I’m ‘addicted’-but because I learned that my body doesn’t have a ‘safe’ setting anymore.
If you’re reading this and you’re still drinking with your meds-please, just pause. For one night. Just one. Ask your pharmacist. Look it up. Don’t wait for your body to scream.
You’re not weak for asking. You’re strong for listening.