Why Renal Ultrasound Is the First Step for Suspected Kidney Blockage
When a patient shows up with severe flank pain, nausea, or decreased urine output, doctors don’t reach for a CT scan right away. They turn to renal ultrasound. It’s fast, safe, and doesn’t expose the patient to radiation. In emergency rooms, hospitals, and even outpatient clinics, this simple imaging test is the go-to tool to check for kidney obstruction and measure kidney size. Why? Because it gives real-time answers without the risks of contrast dye or X-rays. For someone with a suspected kidney stone or urinary blockage, waiting hours for a CT scan isn’t just inconvenient-it’s unnecessary. Renal ultrasound delivers the critical information needed to make the next move: whether to send the patient home with pain meds, admit them for drainage, or schedule further testing.
What Renal Ultrasound Actually Measures
Renal ultrasound doesn’t just take a picture-it measures. The test evaluates several key values that tell doctors if the kidneys are healthy or under pressure. The most important ones are:
- Kidney length: In adults, normal kidneys are 9 to 13 centimeters long. If one kidney is significantly smaller, it may indicate chronic damage or scarring.
- Cortical thickness: The outer layer of the kidney (the cortex) should be at least 1 centimeter thick. Thinning suggests long-standing disease or pressure from blockage.
- Renal pelvis diameter: The central collecting area of the kidney should be less than 7 millimeters wide. Anything wider points to hydronephrosis-urine backing up because of a blockage.
- Resistive index (RI): This is a Doppler-based number that shows how easily blood flows through the kidney’s arteries. A value above 0.70 strongly suggests obstruction. Studies show it’s 87% accurate at spotting blocked urine flow.
These numbers aren’t just for show. They’re used together. A kidney that’s slightly enlarged with a dilated pelvis and an RI of 0.75? That’s a clear sign of acute obstruction. A small, thin-walled kidney with a normal RI? That’s more likely chronic kidney disease.
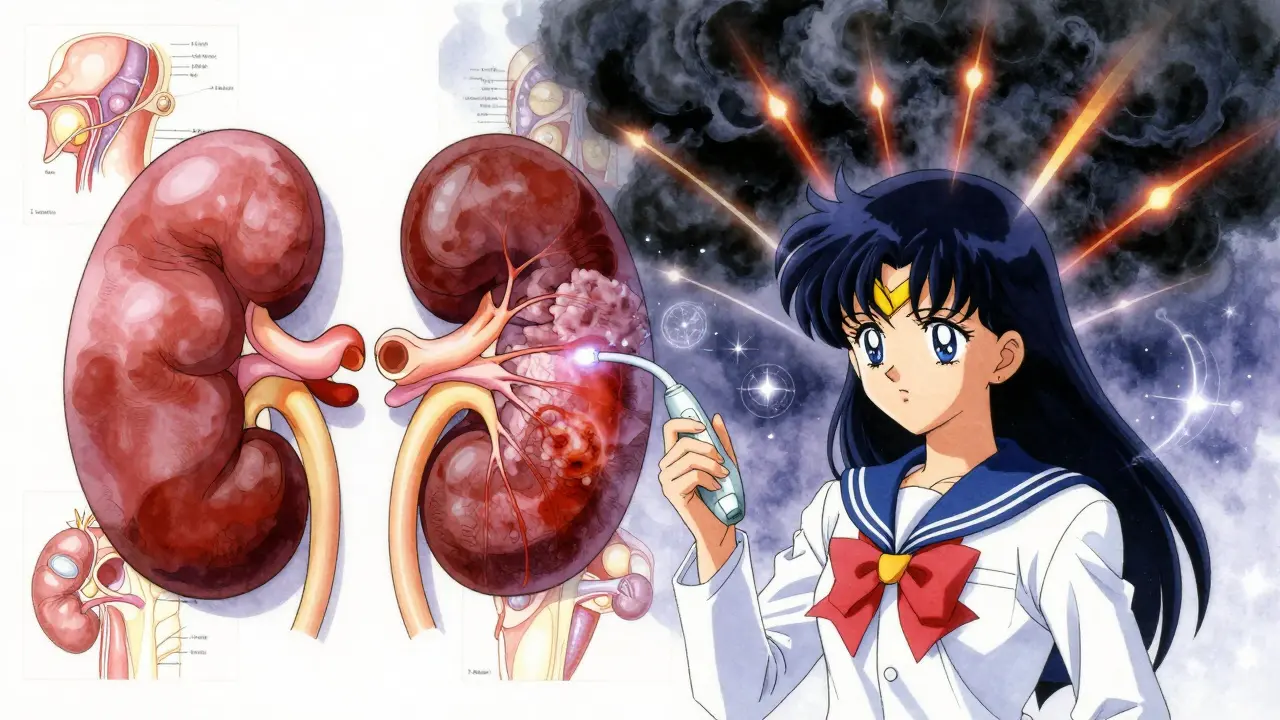
How Ultrasound Finds Obstruction-Even When Stones Aren’t Visible
One of the biggest myths about renal ultrasound is that it’s only good for spotting kidney stones. It’s not. In fact, ultrasound misses about 20% of small stones under 3 millimeters. But here’s the thing: you don’t always need to see the stone to know it’s there.
When a stone blocks the ureter, urine backs up into the kidney. That causes the renal pelvis and calyces to swell-hydronephrosis. Ultrasound picks up that swelling easily. Even if the stone itself is hidden behind bowel gas or too small to see, the backup of urine is unmistakable. That’s why ultrasound is so powerful: it sees the consequence, not just the cause.
Advanced techniques like Doppler ultrasound can also detect abnormal blood flow patterns. In cases of ureteropelvic junction (UPJ) obstruction, for example, the artery feeding the kidney may show a higher resistive index. Some newer systems even use shear-wave elastography to measure how stiff the kidney tissue has become from pressure. Stiffness = obstruction. It’s a direct, physical signal.
Why Ultrasound Beats CT for Initial Screening
CT scans are often seen as the gold standard. And yes, they’re better at finding tiny stones and showing exact anatomy. But they come with a cost: radiation. One CT urogram exposes a patient to about 10 millisieverts of radiation-equivalent to 3 years of natural background exposure. For someone with recurrent kidney stones, that adds up fast. A patient who’s had 5 CT scans in 5 years has absorbed radiation equal to 50 chest X-rays.
Ultrasound avoids that entirely. No radiation. No contrast dye. No need to fast. You can do it at the bedside in under 20 minutes. Emergency departments that use point-of-care ultrasound cut diagnosis time by nearly 45 minutes compared to waiting for formal imaging. That’s not just efficient-it’s lifesaving when a patient is in severe pain or developing sepsis from a blocked kidney.
Guidelines from the American College of Radiology and the American Urological Association both rank renal ultrasound as “usually appropriate” as the first test for suspected obstruction. CT is rated lower-not because it’s worse, but because it’s overkill for a first look.
When Ultrasound Falls Short-And What Comes Next
Ultrasound isn’t perfect. It has limits. In patients with a BMI over 35, sound waves struggle to penetrate deep tissue. The image gets blurry, measurements become unreliable, and the test may need to be repeated with another method.
It also can’t tell you how fast urine is draining from the kidney. That’s where nuclear renal scans come in-they measure function, not just structure. But those involve radiation and take hours. Magnetic resonance urography (MRU) gives detailed 3D images of the urinary tract without radiation, but it’s expensive ($1,500-$2,500), takes longer, and still misses small stones.
So what’s the next step when ultrasound is inconclusive? If hydronephrosis is clear but the cause isn’t, doctors may order a CT scan for stone detection or an MRU if there’s concern about a tumor or stricture. For children or pregnant women, ultrasound remains the only safe option. For older adults with complex anatomy or obesity, CT becomes necessary-but only after ultrasound has done its job.
Who Performs the Test-and Why Skill Matters
Not every ultrasound is created equal. A poorly done exam can miss hydronephrosis or give a false resistive index. Studies show up to 20% variation in kidney size measurements between experienced sonographers and novices. That’s why training matters.
The American Institute of Ultrasound in Medicine (AIUM) recommends at least 40 supervised exams before a sonographer is considered competent. For emergency physicians doing point-of-care scans, it’s even more critical-they need to know exactly where to look and how to interpret subtle signs. A resident who’s done fewer than 50 exams often struggles to measure the resistive index accurately.
Good technique includes:
- Imaging both kidneys in two planes (longitudinal and transverse)
- Measuring the renal pelvis at its widest point, not just the first view
- Using Doppler on the interlobar arteries with a 1mm sample gate
- Getting at least three clean waveforms to calculate RI
- Grading hydronephrosis using the Society for Fetal Urology scale (mild, moderate, severe)
Even small mistakes-like angling the probe too steeply or not hydrating the patient-can change results. That’s why many hospitals now use AI-assisted tools to help standardize measurements and flag potential errors.
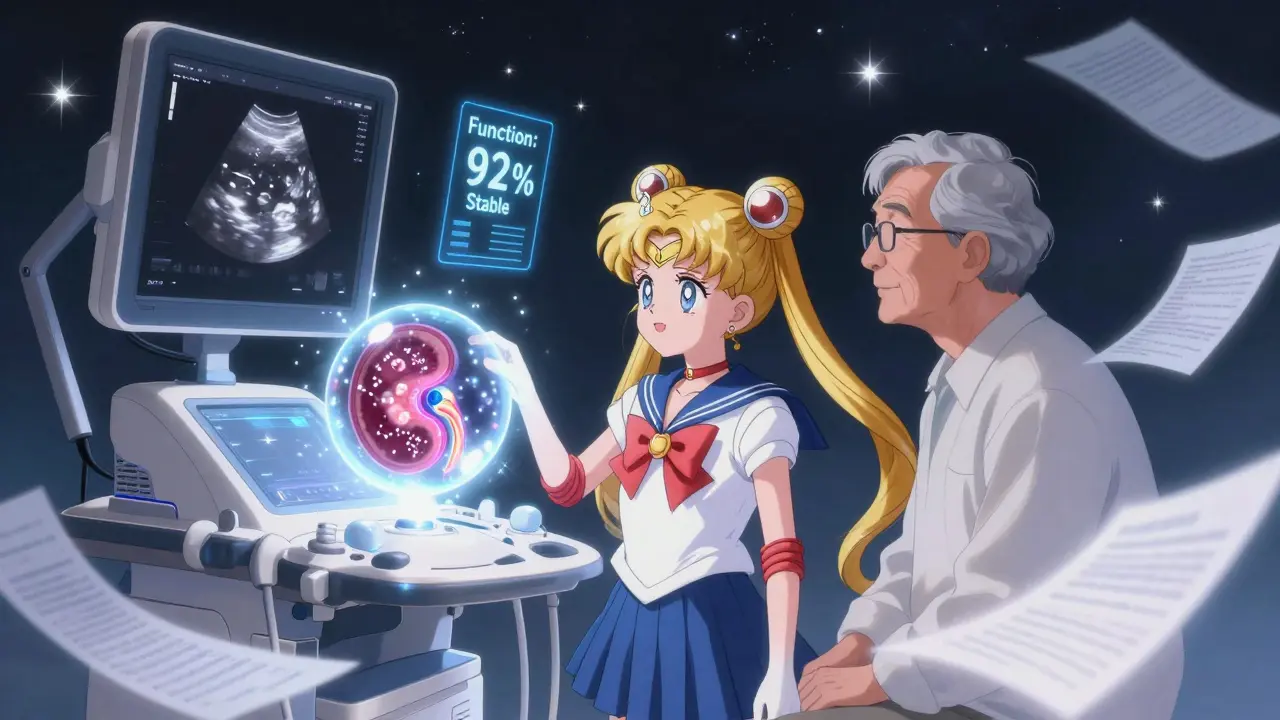
The Future: AI, Super-Resolution, and Quantitative Ultrasound
Ultrasound isn’t standing still. New tech is turning it from a visual tool into a data-rich diagnostic platform. Researchers are now using super-resolution ultrasound to map tiny blood vessels in the kidney-something once only possible with biopsies. This could detect early signs of fibrosis before kidney function drops.
Artificial intelligence is being trained to automatically grade hydronephrosis. Mayo Clinic is testing AI that analyzes ultrasound images and gives a severity score in seconds. Early results show it matches expert readings 92% of the time.
Another breakthrough is ultrasound localization microscopy, which might one day let doctors count individual nephrons-the filtering units of the kidney-without surgery. Imagine knowing how many working filters you have left, just by scanning.
These aren’t sci-fi ideas. They’re in labs and pilot programs right now. Within five years, renal ultrasound won’t just show if a kidney is swollen-it will tell you how much damage has occurred, how much function remains, and how likely it is to recover.
Real-World Use Cases: What This Looks Like in Practice
Here’s how this plays out in real clinics:
- A 42-year-old man with sudden right-sided pain: Ultrasound shows a 10mm dilated renal pelvis, RI of 0.78, and a 5mm stone in the lower ureter. Diagnosis: acute obstruction. He’s given pain relief and scheduled for lithotripsy.
- A 78-year-old woman with urinary retention: Ultrasound reveals bilateral hydronephrosis, thin cortices, and normal RI. No stones. Diagnosis: chronic obstruction from enlarged prostate. She’s referred for urology and catheterization.
- A pregnant woman at 28 weeks with flank pain: CT is off-limits. Ultrasound shows mild hydronephrosis on the right-common in pregnancy. No stone seen, but the pelvis is dilated. She’s monitored weekly. No intervention needed.
- A child with a history of UPJ obstruction: Mom brings him in for a follow-up. Ultrasound shows kidney size unchanged, cortical thickness stable, and RI down from 0.75 to 0.62. The surgery worked. No more blockage.
In each case, ultrasound gave the answer quickly, safely, and accurately. It didn’t need to be fancy. It just needed to be done right.
Final Takeaway: Ultrasound Is the Foundation, Not the Finish Line
Renal ultrasound isn’t the end of the diagnostic journey-it’s the beginning. It’s the tool that tells you whether something’s wrong, how bad it is, and whether you need to act fast. It’s not perfect, but it’s the best first step we have. For patients with suspected obstruction, it’s the difference between unnecessary radiation and a clear path forward. For doctors, it’s the fastest way to rule in or rule out a life-threatening blockage.
As technology improves, ultrasound will get smarter. But its core strengths-speed, safety, accessibility-won’t change. That’s why, in 2026, it’s still the most common kidney imaging test in the world. Over 12 million are done every year in the U.S. alone. And for good reason: it works. When in doubt, start with ultrasound. It’s not just standard practice. It’s smart medicine.


Rachel Liew
February 2, 2026 AT 02:41Aditya Gupta
February 2, 2026 AT 15:03Melissa Melville
February 4, 2026 AT 12:07Lisa Rodriguez
February 4, 2026 AT 12:12franklin hillary
February 6, 2026 AT 01:14Naomi Walsh
February 8, 2026 AT 00:33Ed Di Cristofaro
February 8, 2026 AT 22:56Ishmael brown
February 10, 2026 AT 11:00Donna Macaranas
February 12, 2026 AT 00:11vivian papadatu
February 12, 2026 AT 19:16Deep Rank
February 14, 2026 AT 15:06Bryan Coleman
February 15, 2026 AT 11:42Jamie Allan Brown
February 15, 2026 AT 18:59Lilliana Lowe
February 15, 2026 AT 21:49Jaden Green
February 16, 2026 AT 02:15