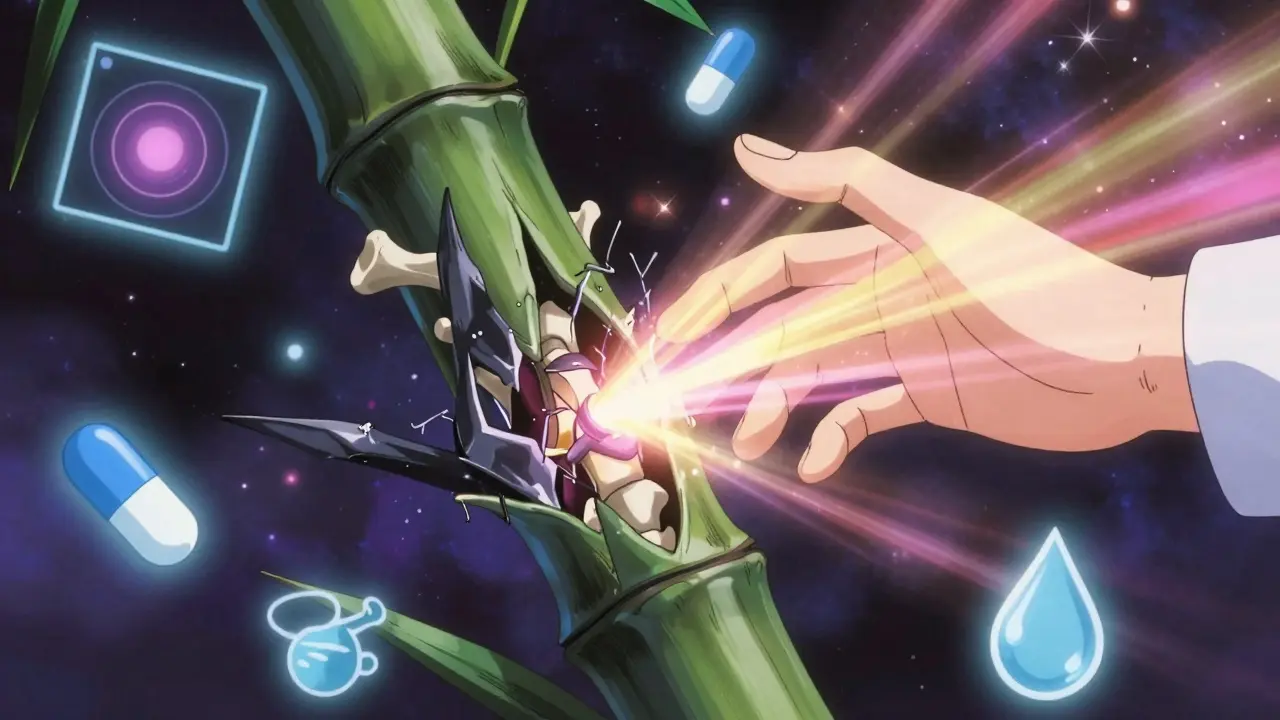
When your back pain doesn’t go away with rest, wakes you up in the early hours, and gets better after you move - that’s not just a bad posture or a pulled muscle. It could be ankylosing spondylitis (AS), a chronic autoimmune condition that slowly fuses your spine. Unlike typical back pain that fades after a few days, AS is a silent thief of movement. It starts with inflammation in the joints where your spine meets your pelvis, and over time, that inflammation builds bone where it shouldn’t. Eventually, your vertebrae can fuse together like a bamboo stalk - a condition called bamboo spine. This isn’t rare. Around 2.7 million people in the U.S. live with it, and most don’t even know they have it for years.
How AS Starts: More Than Just Back Pain
Ankylosing spondylitis doesn’t begin with a fall or a twist. It creeps in. The first sign is usually inflammatory back pain - not the kind you get from lifting heavy boxes, but pain that lasts longer than three months, gets worse at night, and improves with movement. Many people describe waking up between 3 and 6 a.m. with stiffness so bad they can barely roll over. Morning stiffness lasts over 30 minutes, sometimes over an hour. That’s not normal aging. That’s immune system chaos.
The root of AS lies in the entheses - the spots where tendons and ligaments attach to bone. In AS, the immune system attacks these areas, especially in the sacroiliac joints (where your spine connects to your pelvis) and along the spine. Over time, the body tries to heal the damage by laying down new bone. Instead of repairing, it overbuilds. This leads to fusion, loss of flexibility, and in severe cases, a forward-stooped posture. About 30-40% of untreated patients develop full spinal fusion within 10 to 20 years.
Genetics play a huge role. Over 90% of white patients with AS carry the HLA-B27 gene. But having the gene doesn’t mean you’ll get AS - only about 5% of people with HLA-B27 develop it. Still, if you have a family member with AS and you’re experiencing persistent back pain before age 45, you should get checked. It’s not just about the spine, either. AS can also cause eye inflammation (uveitis), Crohn’s disease, psoriasis, and even heart issues. These are clues doctors use to connect the dots.
Diagnosis: Why It Takes Years
On average, people wait over three years to get a correct AS diagnosis. Why? Because most doctors don’t think of it. A patient with back pain is often told they have a herniated disc, sciatica, or even anxiety. One Reddit user shared they saw four doctors before someone finally ordered an MRI. That delay is dangerous. Every year without treatment increases the chance of permanent damage.
Modern diagnosis uses a mix of clinical signs, blood tests, and imaging. The ASAS criteria help doctors spot AS: inflammatory back pain starting before 45, improvement with exercise, no relief with rest, and at least one other feature like uveitis, psoriasis, or a positive HLA-B27 test. Blood tests won’t confirm AS - there’s no single blood marker - but they rule out other conditions. The real game-changer is MRI. Unlike X-rays, which only show damage after bone has changed, MRI can detect inflammation in the sacroiliac joints years before fusion happens. If your MRI shows sacroiliitis and you have inflammatory pain, the diagnosis is clear.
Medications: Controlling the Fire Before It Burns
There’s no cure for AS, but there are tools to stop it from taking over your life. The first line of defense is NSAIDs - drugs like ibuprofen or naproxen. They’re not just for pain. Studies show that consistent NSAID use can cut radiographic progression by half over two years. That’s huge. It means you might avoid fusion if you take them regularly, not just when you’re in pain.
If NSAIDs aren’t enough, biologics come next. These are targeted drugs that block specific parts of the immune system driving inflammation. TNF inhibitors like adalimumab (Humira) and etanercept (Enbrel) have been the go-to for over a decade. They work for 40-60% of patients, with symptom relief often seen within weeks. Newer options like IL-17 inhibitors (secukinumab, ixekizumab) and JAK inhibitors (upadacitinib) are showing even better results. In the SELECT-AXIS 1 trial, upadacitinib helped 45% of patients achieve major symptom improvement in just 14 weeks.
But these drugs aren’t cheap. Without insurance, biologics can cost $5,000 to $6,000 a month. That’s why many patients delay starting them - and that’s where things get risky. Experts now argue that waiting until NSAIDs fail might be too late. Early use of biologics, especially in young patients with high inflammation, can prevent structural damage before it’s irreversible.
Mobility: The Most Powerful Treatment You Can Do Yourself
Medications slow the disease. Exercise stops the fusion. That’s the truth. Physical therapy isn’t optional - it’s essential. Studies show structured daily exercise improves spinal mobility by 25-30% in just six months. That’s not a small gain. That’s the difference between bending over to tie your shoes and not being able to at all.
The gold standard is a program that includes:
- Deep breathing exercises to keep the rib cage flexible
- Spinal extension stretches - lying on your stomach, lifting your chest
- Shoulder rolls and chest openers to prevent hunching
- Aquatic therapy - swimming or water aerobics reduces joint stress
- Posture training - sitting upright, standing tall, sleeping on a firm mattress
One patient in Leeds, who started swimming 45 minutes a day, cut her morning stiffness from 90 minutes to 20 minutes in three months. That’s not magic - it’s physics. Movement keeps the joints lubricated, prevents scar tissue from forming, and maintains muscle strength around the spine. Even during flares, gentle motion matters. Try pelvic tilts in bed before you get up. Stretch your arms overhead while lying down. Don’t wait until you feel better to move - move to feel better.
Adherence is the biggest hurdle. Only 45% stick with daily exercise after one month. But with digital trackers - apps that log your stretches, send reminders, or even use video feedback - adherence jumps to 78% after six months. Your spine doesn’t care if you feel motivated. It only responds to consistent motion.
Living with AS: Daily Adjustments That Make a Difference
AS doesn’t just attack your spine - it reshapes your life. Fatigue is the most common complaint, reported by 74% of patients. It’s not laziness. It’s inflammation. Work becomes harder. Sitting for long hours? That’s a trigger. Standing all day? That’s pain. Many need workplace accommodations - standing desks, flexible hours, or remote options.
Small changes make big differences:
- Sleep on your back with a thin pillow - or no pillow - to keep your spine straight
- Use a lumbar roll in your chair to avoid slouching
- Wear supportive shoes - no flip-flops
- Take movement breaks every 30 minutes, even if it’s just standing up and rolling your shoulders
- Heat therapy before exercise - a warm shower or heating pad for 20 minutes loosens stiff joints
Yoga and tai chi are also powerful tools. Johns Hopkins offers AS-specific yoga routines that focus on spinal alignment and controlled breathing. These aren’t just relaxation techniques - they’re functional training for your spine.
What’s Next: New Hope on the Horizon
The future of AS care is getting brighter. The FDA approved upadacitinib (Rinvoq) in 2023 - the first JAK inhibitor for AS. It’s oral, not injected, and works fast. Research published in Nature Reviews Rheumatology shows IL-17 inhibitors can reduce bone growth by 55% over two years. That’s not just symptom control - it’s disease modification.
Meanwhile, the STABILITY trial is testing whether 150 minutes of moderate-to-vigorous exercise per week (like brisk walking, cycling, or swimming) is better than standard recommendations. Early results suggest it cuts spinal fusion risk by 30%. This isn’t theory - it’s real data from 500 patients across 35 U.S. centers.
The global market for AS treatments is growing fast, expected to hit $22.6 billion by 2028. That means more research, more options, and more access. But the biggest breakthrough isn’t a drug. It’s awareness. When patients learn early, when doctors recognize the signs, and when movement becomes as routine as brushing your teeth - AS stops being a sentence. It becomes a condition you manage.
What You Can Do Today
If you’ve had back pain for more than three months, especially if it wakes you up at night and improves with movement:
- See a rheumatologist - not just your GP
- Ask for an MRI of your sacroiliac joints
- Start daily stretching - even if it’s just 10 minutes
- Track your symptoms with an app or journal
- Join a patient group - like the Spondylitis Association of America - for free exercise videos and support
You don’t have to live with stiffness. You don’t have to accept fusion. With the right combination of medicine and movement, you can keep your spine - and your life - moving.
Can ankylosing spondylitis be cured?
No, there is no cure for ankylosing spondylitis. But it can be managed effectively. With early diagnosis, consistent medication, and daily exercise, most people prevent spinal fusion and maintain full mobility for decades. The goal isn’t to eliminate the disease - it’s to stop it from taking over your life.
Is ankylosing spondylitis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) mainly attacks the small joints in the hands and feet and is usually seropositive - meaning it shows up in blood tests as rheumatoid factor or anti-CCP antibodies. Ankylosing spondylitis affects the spine and sacroiliac joints, is typically seronegative (no markers in blood), and is strongly linked to the HLA-B27 gene. RA causes joint erosion; AS causes bone fusion.
Do I need to take medication for life?
Not necessarily. Some people can reduce or stop medication after years of stable disease, especially if they maintain daily exercise and have low inflammation markers. But stopping without medical guidance can lead to flare-ups and damage. Always work with your rheumatologist. Many patients stay on low-dose NSAIDs long-term for prevention, even if they stop biologics.
Can exercise make ankylosing spondylitis worse?
Only if you push too hard during a flare. Gentle, consistent movement is safe and essential. High-impact activities like running or heavy weightlifting might irritate inflamed joints, but swimming, yoga, and stretching are protective. If pain increases after exercise, reduce intensity - don’t stop. The key is finding the right balance between challenge and comfort.
Why does AS cause fatigue?
Fatigue in AS isn’t from lack of sleep - it’s from chronic inflammation. Inflammatory cytokines like IL-6 and TNF-alpha affect your brain’s energy centers, making you feel drained even after a full night’s rest. This is biological, not psychological. Managing inflammation through medication and exercise often improves fatigue more than caffeine or naps.
What happens if I stop exercising?
If you stop daily movement, your spine stiffens quickly. Within weeks, mobility declines. Within months, the risk of fusion increases. Exercise doesn’t just relieve pain - it physically prevents bone growth in the wrong places. Think of it like brushing your teeth: skipping it doesn’t cause instant damage, but over time, it leads to irreversible consequences.


Jason Pascoe
February 12, 2026 AT 12:36Had AS for 12 years now. NSAIDs saved my life, but honestly? The swimming routine changed everything. Used to be stuck in bed until noon. Now I’m up, stretched, and in the pool by 7 a.m. No magic pill - just consistency. My spine still hates me, but it doesn’t own me anymore.
Sonja Stoces
February 13, 2026 AT 21:07LMAO at ‘exercise stops fusion’ like it’s some yoga cult. I’ve got bamboo spine and I’ve been ‘stretching’ for 8 years. My MRI looks like a fossil. Biologics work. Period. Stop pretending movement is a cure. 😂
Rob Turner
February 15, 2026 AT 03:22Been here since 2019. UK NHS was slow as hell, but finally got my MRI after begging. That moment? When the radiologist said ‘sacroiliitis’? Felt like I’d been screaming into a void and someone finally heard me.
Also - yes, the HLA-B27 thing is wild. I’ve got it. My dad’s got it. My sister doesn’t. Genetics is a gamble with your spine. 🤷♂️
Luke Trouten
February 15, 2026 AT 09:46There’s a subtle but critical point here: AS isn’t just about pain management. It’s about preserving function before the body overcompensates. The fusion isn’t pain itself - it’s the loss of autonomy. That’s why early intervention isn’t just medical advice - it’s a preservation of identity. Movement isn’t therapy. It’s self-defense.
Jonathan Noe
February 16, 2026 AT 08:40Y’all are underestimating the JAK inhibitors. Upadacitinib? Game-changer. I was on Humira for 3 years - barely moved. Switched to Rinvoq in January. By week 6? I could tie my shoes without groaning. And it’s a pill. No needles. No $6k/month. My insurance barely blinked. If you’re on biologics and not seeing progress, ask your rheum about JAKs. Seriously.
Jim Johnson
February 17, 2026 AT 07:33Just started my daily stretches last week. 10 minutes before bed - pelvic tilts, cat-cow, deep breaths. Didn’t think it’d do anything. But yesterday? I rolled over in bed without wincing. For the first time in 5 years.
Also, the heating pad trick? Genius. I use my microwaveable rice bag. Smells like cinnamon. Feels like hope.
PS: I joined the Spondylitis Association. Their YouTube channel is a lifesaver. Free, no ads, just real people doing real moves.
Vamsi Krishna
February 18, 2026 AT 17:35Bro, you think AS is bad? I got AS + psoriatic arthritis + uveitis + Crohn’s. My body’s basically a warzone. I’ve been on 7 meds. Lost 3 jobs. My wife left. I’m 29. You wanna talk about ‘silent thief’? Nah. It’s a goddamn thief with a crowbar.
But here’s the thing - I swim every morning. 10 laps. No excuses. Even when I can’t walk. Even when my eyes are red. Because if I stop, I die slow. So I move. And I’m still here. You wanna live? Move. Not ‘maybe’. MOVE.
Pat Mun
February 20, 2026 AT 08:22I used to think AS was just ‘old people back pain’ until I saw my cousin’s X-rays. Her spine looked like a stack of bricks glued together. She’s 38.
What nobody talks about? The fatigue. It’s not laziness. It’s like your bones are full of wet cement. I nap three times a day. My boss thinks I’m lazy. I showed her the research. Now she lets me work from home.
Also - yoga. Not the bendy kind. The AS-specific stuff. Johns Hopkins has a 15-minute routine. I do it while my coffee brews. Changed. My. Life.
And yes - sleeping on your back with no pillow? Sounds insane. Works. I used to wake up with my neck bent sideways. Now? I sleep like a normal human. 🙏
Reggie McIntyre
February 20, 2026 AT 09:48AS is the ultimate ‘invisible illness’ - you look fine. You’re not. I got diagnosed after my dog started whining when I got out of bed. He knew something was off.
My rheumatologist said: ‘If you’re not sweating after stretching, you’re not doing it right.’ I thought he was joking. He wasn’t. Now I do 45 mins of water aerobics 5x a week. My joints feel like they remember how to bend.
And the apps? I use ‘Mobility Tracker’. It pings me. I hate it. But it works. I’ve done 87 days straight. No breaks. My spine is mad at me… but it’s still mobile. That’s the win.
Stacie Willhite
February 21, 2026 AT 18:42I just want to say thank you for writing this. I’ve been silent for years. Scared. Ashamed. Thought I was just ‘weak’.
My husband thought I was being dramatic. Then he saw the MRI. He cried. We started stretching together last week. He does it with me. Even though he doesn’t have AS.
It’s not about the spine. It’s about not being alone. You’re not alone. I’m here. We’re all here.
Annie Joyce
February 22, 2026 AT 22:30My doc said ‘take NSAIDs daily’ and I laughed. Like, who does that? But I did. For 3 months. No pain. No flares. Just… normal. I didn’t even realize how much pain I was living in until it was gone.
Also - no flip-flops. Ever. I bought these orthopedic sandals. Look like alien shoes. My feet are happy. My spine thanks me.
And yes - I cry during stretches sometimes. It’s not weakness. It’s release. I’m allowed.
Gabriella Adams
February 24, 2026 AT 04:45While the clinical data is compelling, we must not reduce human experience to biomarkers and radiographic progression. The lived reality of ankylosing spondylitis is one of existential recalibration - a recalibration not merely of posture, but of identity, autonomy, and the very architecture of daily life. The spine, once taken for granted, becomes a monument to vulnerability. And yet, within that vulnerability lies a profound resilience - not in spite of the disease, but through the deliberate, daily reclamation of motion. Movement, therefore, is not therapy - it is reclamation.
Kristin Jarecki
February 25, 2026 AT 19:50It is imperative to emphasize that early diagnosis and intervention are not merely clinical best practices - they are ethical imperatives. The irreversible nature of spinal fusion necessitates a proactive, multidisciplinary approach that prioritizes patient autonomy, access to imaging, and equitable pharmaceutical coverage. Delayed care is not negligence - it is structural violence.
Brad Ralph
February 26, 2026 AT 07:23So… we’re all just gonna stretch our way out of fused vertebrae? 😏