Colchicine Dosing Calculator for Gout Treatment
This tool helps determine the appropriate colchicine dosage based on kidney function, age, and potential drug interactions. Always follow your healthcare provider's instructions.
How to Use This Tool
1. Select your kidney function level 2. Enter your age 3. Check any medications that may interact with colchicine 4. Choose if this is for acute flare treatment or prevention 5. Click "Calculate" for your recommended dose
Recommended Dosage
When a gout flare hits, the burning pain can feel like a firecracker in your big toe. Colchicine is a centuries‑old drug that steps in to calm that fire. It isn’t a steroid, it isn’t an NSAID, and it doesn’t lower uric acid levels - it works by pulling the plug on the cellular fireworks that cause the swelling. Below we break down exactly how colchicine does that, what you should know before you take it, and how it compares to other gout medicines.
What is gout, and why does it flare?
Gout is a form of inflammatory arthritis caused by the buildup of monosodium urate crystals in joints. When uric acid in the blood spikes - often after a binge on red meat, beer, or sugary drinks - the excess crystallises. The crystals act like tiny needles that irritate the lining of the joint, especially the first metatarsophalangeal joint (the big toe). The body’s immune system sees these crystals as an invader and floods the area with white blood cells, leading to the classic redness, swelling, and excruciating pain.
Where does colchicine fit in the gout treatment ladder?
In clinical practice, gout attacks are usually tackled in three steps:
- Rapid pain control (NSAIDs, steroids, or colchicine).
- Preventing future flares (allopurinol, febuxostat, lifestyle changes).
- Managing complications (kidney stones, chronic joint damage).
Colchicine belongs to the first step. It’s especially useful when NSAIDs are contraindicated - for example, in people with stomach ulcers or kidney issues. Because it works on a different pathway, doctors often prescribe it alongside other drugs to cover all bases.
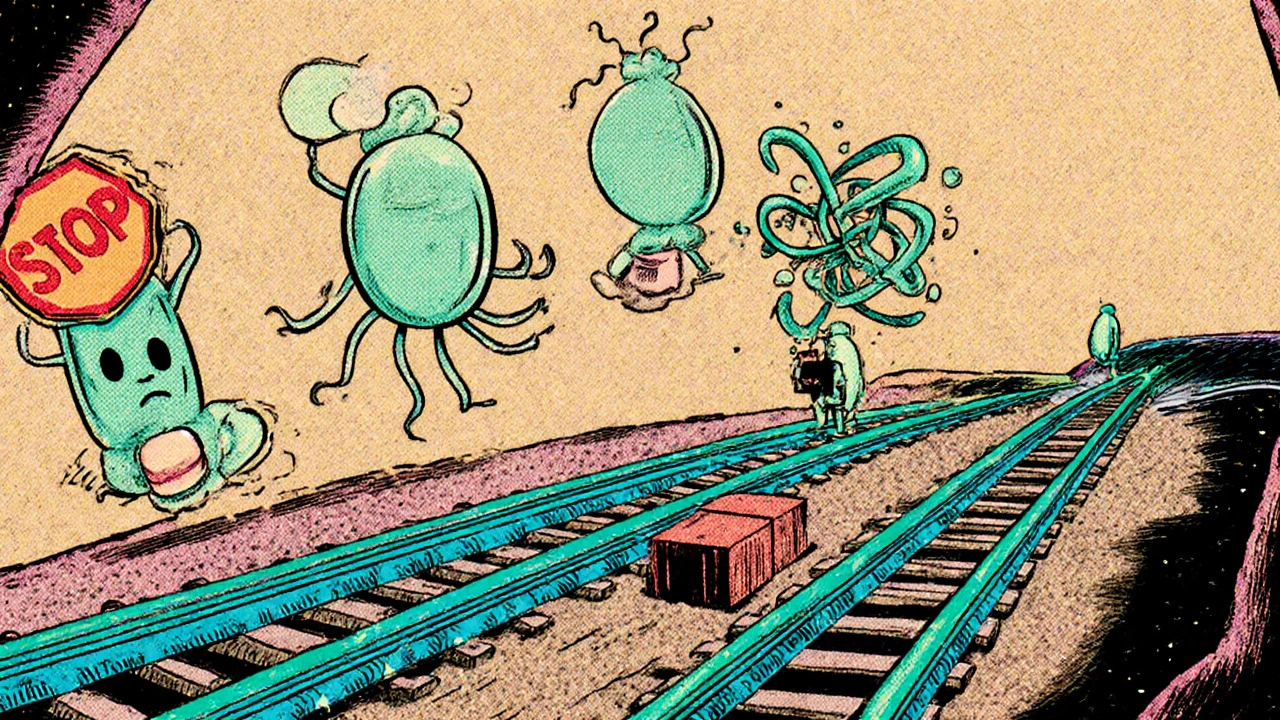
How does colchicine stop the pain? The microtubule story
The magic begins inside a cell’s skeleton. Every cell contains tiny tubes called microtubules. They act like railroad tracks, guiding vesicles, organelles, and even the movement of immune cells. Colchicine binds to a protein called tubulin, a building block of microtubules, and prevents the tubes from forming. Think of it as freezing the tracks - without functional microtubules, white blood cells (especially neutrophils) can’t migrate to the crystal‑laden joint efficiently.
When neutrophils can’t reach the site, they can’t release the compounds that amplify inflammation. This halts the cascade early, reducing swelling and pain within a few hours of the first dose.
The inflammasome pathway - colchicine’s second strike
Beyond blocking cell movement, colchicine tampers with a molecular alarm system called the inflammasome. The most studied inflammasome in gout is the NLRP3 complex, which senses the presence of urate crystals. When activated, NLRP3 triggers the production of interleukin‑1β (IL‑1β), a potent cytokine that drives fever, pain, and swelling.
Colchicine interferes with two key steps:
- It prevents the assembly of the NLRP3 complex by disrupting the microtubule‑dependent transport of the adaptor protein ASC (apoptosis‑associated speck‑like protein).
- It inhibits the activation of pyrin, another sensor that can boost IL‑1β release in response to certain bacterial toxins.
The net result is a far lower surge of IL‑1β, meaning the joint’s pain‑signalling pathways stay quiet.
Pharmacokinetics you should know
Colchicine is absorbed quickly from the gut - peak blood levels appear in about 1‑2hours. It’s metabolised mainly by the liver enzyme cytochromeP4503A4 and cleared by the kidneys. Because of this dual route, two things matter a lot:
- Renal function: If your kidneys work at less than 50% of normal, the drug can build up, raising the risk of toxicity (diarrhoea, muscle pain, even bone‑marrow suppression).
- Drug interactions: Strong CYP3A4 inhibitors (like clarithromycin or grapefruit juice) can push colchicine levels too high. Likewise, P‑glycoprotein inhibitors (such as verapamil) have a similar effect.
For most adults, the standard acute‑gout regimen is 1.2mg (often two 0.6mg tablets) followed by 0.6mg one hour later, then 0.6mg once or twice daily for the next 24‑48hours. Doctors may halve the dose for patients over 70, those with renal impairment, or anyone taking CYP3A4‑interacting meds.
Colchicine vs. other acute gout meds: a quick look
| Medication | Primary Action | Typical Onset | Key Contra‑indications | Common Side‑effects |
|---|---|---|---|---|
| Colchicine | Microtubule inhibition & inflammasome suppression | 1‑2hrs | Severe renal/hepatic failure, CYP3A4 inhibitors | Diarrhoea, nausea, muscle pain |
| NSAIDs (e.g., Indomethacin) | Cyclo‑oxygenase inhibition → ↓ prostaglandins | 30‑60mins | Peptic ulcer, renal insufficiency, heart failure | Stomach upset, headache, renal toxicity |
| Corticosteroids (e.g., Prednisone) | Broad anti‑inflammatory (NF‑κB suppression) | 4‑6hrs | Uncontrolled diabetes, active infection, osteoporosis | Weight gain, mood changes, glucose rise |
Notice how colchicine’s onset sits between NSAIDs (fast) and steroids (slower). Its side‑effect profile is mostly gastrointestinal, while NSAIDs threaten the stomach and kidneys, and steroids bring systemic hormonal effects.
Safety tips and red flags
Even though colchicine is an old drug, misuse can be dangerous. Keep these pointers in mind:
- Never exceed the prescribed dose. Toxic levels can cause severe bone‑marrow suppression, leading to low blood counts.
- Watch for persistent diarrhoea. If it lasts more than 48hours, contact a pharmacist - dehydration can worsen kidney function.
- Inform every prescriber that you’re on colchicine, especially before starting antibiotics, antifungals, or heart medications.
- Pregnancy & breastfeeding: Use only if the doctor says the benefits outweigh the risks. Animal studies suggest high doses can affect fetal development.
When colchicine isn’t enough - stepping up therapy
If attacks keep coming despite colchicine, the next move is usually a urate‑lowering drug. Allopurinol and febuxostat block the production of uric acid, preventing crystal formation in the first place. In refractory cases, biologics that target IL‑1β directly, such as canakinumab, can be prescribed.
Remember: colchicine only treats the flare; it does not cure gout. Long‑term management always includes diet tweaks (limit organ meat, limit alcohol), hydration, and weight control.
Quick reference checklist for patients
- Take the first dose as soon as pain starts - earlier means less swelling.
- Stay hydrated; aim for at least 2L of water per day.
- Avoid grapefruit juice while on colchicine.
- If you have chronic kidney disease, ask your doctor about a reduced dose.
- Keep a symptom diary: note onset, dosage, and side‑effects to discuss at the next appointment.
Frequently Asked Questions
Can I take colchicine with NSAIDs?
Yes, many doctors prescribe a short NSAID course alongside colchicine for extra pain control, as long as you have no stomach or kidney issues. Always follow the dosing schedule your prescriber gives you.
How long does a colchicine course last?
For an acute flare, the typical regimen is 1.2mg then 0.6mg an hour later, followed by 0.6mg one or two times daily for the next 24‑48hours. Some clinicians use a shorter 2‑dose schedule to reduce gastrointestinal side‑effects.
Is colchicine safe for older adults?
Older adults can use colchicine, but the dose is usually halved because kidney function tends to decline with age. Your doctor will check your creatinine clearance before prescribing.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s less than 4hours until the next scheduled dose. In that case, skip the missed one to avoid overdose.
Can colchicine be used for chronic gout prevention?
Low‑dose colchicine (0.6mg once or twice a week) is sometimes prescribed for chronic prevention, especially when urate‑lowering drugs are not tolerated. This regimen keeps the inflammasome in check without the high‑dose side‑effects.
Understanding how colchicine works empowers you to use it wisely, avoid pitfalls, and combine it with lifestyle changes that keep the uric acid monster at bay. If you’re unsure about dosing, side‑effects, or drug interactions, a quick chat with your pharmacist or rheumatologist can save you a lot of hassle.


Tesia Hardy
October 16, 2025 AT 17:43Hey folks, just wanted to say great post! Colchicine can be a real lifesaver when a gout flare hits out of nowhere. Remember to start the first dose as soon as the pain kicks in, that way you can keep the swelling down faster. Also, keep an eye on your kidneys if you have any issues, the drug can stick around longer than you think. Stay hydrated and you’ll be on the mend before you know it.
Matt Quirie
October 25, 2025 AT 04:30Indeed, the information presented is quite comprehensive; however, I would like to emphasize the importance of monitoring renal function, especially in older patients; dosage adjustments are frequently necessary, and clinicians should remain vigilant for potential drug‑drug interactions.
Pat Davis
November 2, 2025 AT 14:16From a clinical standpoint, the mechanistic explanation of colchicine’s impact on the NLRP3 inflammasome is particularly valuable. It clarifies why the drug can be effective even when NSAIDs are contraindicated. I also appreciate the clear dosage guidelines, which aid in avoiding toxicity. Furthermore, the comparison table succinctly highlights its position among acute gout therapies.
Mary Wrobel
November 11, 2025 AT 01:03Absolutely! The way you broke down the microtubule inhibition felt like a vivid picture in my mind. I love the analogy of “freezing the tracks" – it makes the science relatable. And those practical tips, like steering clear of grapefruit juice, are pure gold for anyone on colchicine.
Michelle Guatato
November 19, 2025 AT 11:50They don’t tell you that colchicine is actually a secret weapon from the pharma elite.
Gabrielle Vézina
November 27, 2025 AT 22:36Listen, the drama surrounding colchicine is far deeper than most admit. The drug has been around for centuries yet its true power is hidden. It silently commandeers the cellular highways, halting the immune soldiers before they can even see the enemy. By sabotaging the NLRP3 inflammasome it stops the fire before it sparks. This is not a simple painkiller; it is a molecular saboteur. The body’s own defenses are turned off like a light switch. Imagine the chaos if this switch were flipped the other way. The cascade of IL‑1β would roar like a volcano. Researchers have uncovered this secret and yet the mainstream narrative stays dull. The tables in the article do not capture the magnitude of this maneuver. Every dose is a calculated strike against inflammation, a silent war inside your joints. Side‑effects like diarrhea are merely the casualties of battle, not failures. Renal clearance is another frontline, and those with kidney issues become vulnerable targets. The interplay with CYP3A4 is a covert alliance, making some patients walk a razor’s edge. In short, colchicine is a double‑edged sword, a hero and a villain wrapped in one pill.
Patricia Fallbeck
December 6, 2025 AT 09:23One must concede that the article achieves a commendable synthesis of pharmacology and practical guidance. The prose, while accessible, does not sacrifice rigor, a balance often elusive in patient‑focused literature. It is evident that the author possesses a refined understanding of gout’s pathophysiology. 🧐📚
Brett Snyder
December 14, 2025 AT 20:10Well, I cantsaid it widout a lil bit of patriotic pride – this drug helped many of our folks keep fighting, especially when the sierra resorts tarnish our health. I tought we should shout it out loud, not hide it.
Nidhi Jaiswal
December 23, 2025 AT 06:56Colchicine is useful for acute gout attacks. Take it early and stay hydrated. Avoid grapefruit juice while on the medication.
Sunil Sharma
December 31, 2025 AT 17:43Thanks for the clear points! Starting early really does make a difference, and staying hydrated is a simple yet effective tip. I’ll be sure to remind my patients about drug interactions, especially with antibiotics.
Leah Robinson
January 9, 2026 AT 04:30Loving the thoroughness of this rundown. It’s nice to see the science broken down without the jargon overload. The checklist at the end is super handy for anyone dealing with a flare. Keep the good vibes coming! 😊
Abhimanyu Lala
January 17, 2026 AT 15:16Short and sweet – start early, stay hydrated.