Pneumonia vs. Bronchitis Symptom Checker
Answer These Questions
Select all symptoms you're experiencing. This tool helps identify potential respiratory conditions based on article information.
Quick Summary
- Pneumonia and bronchitis are both lung infections that often share the same germs.
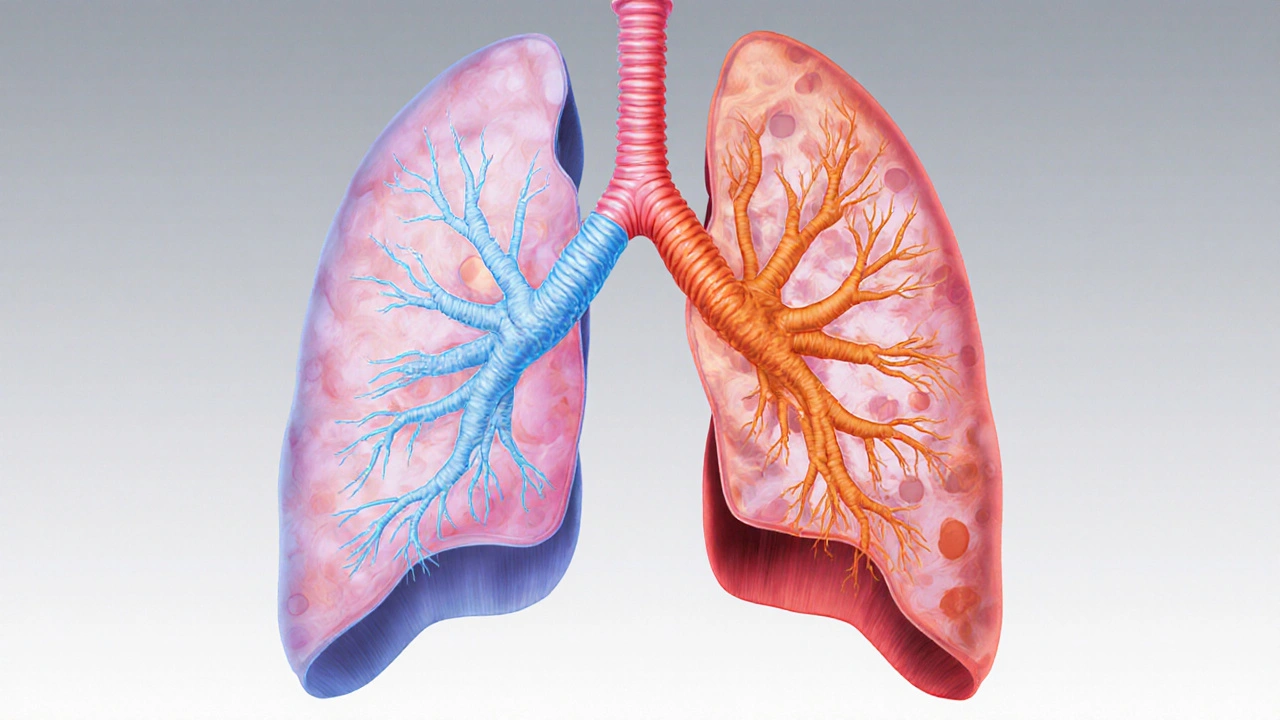
- Bronchitis affects the airways; pneumonia reaches the lung tissue itself.
- Smoking, weak immunity, and chronic lung disease raise the chance of one turning into the other.
- Chest X‑ray and sputum tests are the quickest ways to tell them apart.
- Vaccines, hand‑washing, and quitting smoking cut the risk for both.
What Is Pneumonia?
When you see Pneumonia is an infection that inflames the air sacs (alveoli) in one or both lungs, filling them with fluid or pus. The condition can be sparked by bacteria, viruses, or fungi, and it often brings fever, chills, shortness of breath, and a deep, hacking cough.
According to the World Health Organization, pneumonia accounts for about 15% of all deaths in children under five worldwide, highlighting how serious the disease can be when left untreated.
What Is Bronchitis?
Bronchitis is the inflammation of the bronchial tubes that carry air to and from the lungs. It usually shows up as a persistent cough that produces mucus, along with wheezing and mild fever.
Bronchitis comes in two flavors: acute, which lasts a few weeks and often follows a cold, and chronic, which persists for at least three months each year over two consecutive years. Chronic bronchitis is a key component of chronic obstructive pulmonary disease (COPD).
How the Two Conditions Interact
Both diseases belong to the broader family of respiratory infections. They share many triggers-most notably bacteria like Streptococcus pneumoniae and viruses such as influenza. When the lining of the bronchial tubes is already irritated by bronchitis, the same germs can slip deeper into the alveoli, sparking pneumonia.
Risk factors such as smoking, exposure to air pollutants, and a weakened immune system act as a bridge between the two conditions. For example, a smoker’s cilia (tiny hair‑like structures that clear mucus) are damaged, making it easier for pathogens to travel from the bronchi to the lung tissue.
When Bronchitis Turns Into Pneumonia
In many clinical cases, a bout of acute bronchitis is the first stage of a bacterial or viral cascade. If the immune response fails to clear the invader, the infection can spread to the alveoli, resulting in secondary pneumonia. This progression explains why doctors often warn patients with persistent coughs to watch for new symptoms like sharp chest pain, high fever, or a sudden drop in oxygen levels.
Studies from the American Thoracic Society in 2023 showed that about 12% of adults hospitalized for community‑acquired pneumonia had a documented recent episode of bronchitis, underscoring the link.
How Doctors Distinguish Between the Two
Physical exam findings overlap, but a few tools help separate them:
- Chest X‑ray - A chest X‑ray reveals infiltrates in the lung tissue for pneumonia, while bronchitis may show a clear lung field.
- Sputum analysis - Culturing the mucus can identify the exact virus or bacteria responsible.
- Blood tests - Elevated white‑blood‑cell counts point more toward bacterial pneumonia.
These diagnostics guide treatment decisions, which differ in antibiotic use and supportive care.
Treatment Overlap and Differences
Both conditions benefit from rest, hydration, and fever‑reducing medications like acetaminophen. However:
- Pneumonia - If bacterial, doctors prescribe antibiotics such as amoxicillin or macrolides for 7‑10 days. Viral pneumonia may only need antivirals (e.g., oseltamivir for flu) and close monitoring.
- Bronchitis - Acute cases are usually viral, so antibiotics are avoided unless a bacterial superinfection is confirmed. Chronic bronchitis treatment focuses on bronchodilators, steroids, and pulmonary rehab.
Because the line can blur, clinicians sometimes start a short course of antibiotics if pneumonia can’t be ruled out, especially in high‑risk patients.

Preventing Both Conditions
Prevention strategies hit the shared risk factors head‑on:
- Vaccination - The flu shot and pneumococcal vaccine dramatically lower the odds of catching the germs that cause severe pneumonia and secondary bronchitis.
- Hand hygiene - Regular washing removes pathogens before they can be inhaled.
- Smoking cessation - Quitting restores ciliary function and reduces chronic airway inflammation.
- Air quality - Using air purifiers and avoiding smoky or dusty environments lowers exposure.
People with chronic diseases like COPD or heart failure should get annual flu vaccinations and discuss pneumococcal boosters with their doctors.
Key Differences at a Glance
| Aspect | Pneumonia | Bronchitis |
|---|---|---|
| Primary site | Alveoli (lung tissue) | Bronchial tubes (airways) |
| Typical cause | Bacterial, viral, fungal | Mostly viral; bacterial in chronic cases |
| Key symptoms | High fever, chills, chest pain, shortness of breath | Persistent cough, mucus production, wheezing |
| Diagnostic tool | Chest X‑ray showing infiltrates | Clinical exam; X‑ray often normal |
| Treatment | Antibiotics (if bacterial), antivirals, oxygen | Bronchodilators, steroids, antibiotics only if bacterial |
| Complication risk | High - can lead to sepsis, respiratory failure | Moderate - can progress to pneumonia |
Bottom Line
The link between pneumonia and bronchitis lies in shared germs, common risk factors, and the way inflammation can spread from the airways into the lung tissue. Understanding the difference helps you catch severe symptoms early, get the right tests, and follow a treatment plan that prevents complications.
Frequently Asked Questions
Can a cold cause pneumonia?
A simple cold usually stays in the upper airway, but if the virus spreads to the lower lungs, it can trigger pneumonia, especially in people with weak immune systems.
Do antibiotics work for bronchitis?
Most acute bronchitis is viral, so antibiotics aren’t needed. They’re prescribed only when a bacterial superinfection is confirmed or if the patient is high‑risk.
What symptoms tell me bronchitis has become pneumonia?
Watch for sharp chest pain that worsens with deep breaths, a high fever above 101°F, rapid breathing, or a sudden drop in oxygen saturation. These signs usually prompt a chest X‑ray.
Are there vaccines that protect against both conditions?
The flu vaccine protects against influenza, a common trigger for both bronchitis and viral pneumonia. The pneumococcal vaccine shields against Streptococcus pneumoniae, a leading bacterial cause of pneumonia and secondary bronchitis.
How long does it take to recover from pneumonia?
Recovery varies. Mild cases may improve in a week with proper antibiotics, while severe pneumonia can require weeks of rest and possibly rehabilitation to regain full lung function.

Claire Kondash
October 13, 2025 AT 21:07When we contemplate the delicate dance between pneumonia and bronchitis, we are reminded that the human body is a microcosm of interlinked systems, each whispering the story of health and vulnerability 😊. The article wisely highlights shared pathogens, yet the philosophical nuance lies in recognizing how inflammation, like a restless mind, can migrate from the bronchi to the alveoli, altering the very essence of respiration. Consider the cilia as tiny philosophers, tirelessly sweeping away irritants; when they falter, the narrative of infection expands, bridging bronchial irritation to pulmonary invasion. Smoking, as the author notes, stains this tale with toxic ink, damaging those microscopic sentinels and paving a treacherous path for bacteria to infiltrate deeper layers. Vaccination, in this metaphor, becomes a beacon of enlightenment, illuminating the immune system's capacity to preempt these stories before they unfold.
Moreover, the diagnostic tools-chest X‑rays and sputum cultures-serve as the empirical lenses through which clinicians decipher the hidden chapters of disease. The differentiation between infiltrates and clear fields is not merely a clinical checkpoint but an epistemological separation of truth from illusion. Treatment parallels moral philosophy: antibiotics, when rightly prescribed, act as virtuous agents restoring balance, whereas their misuse can breed resistance, akin to hubris leading to downfall.
In the grand tapestry of respiratory health, the overlap of pneumonia and bronchitis reminds us that boundaries are fluid, and vigilance, akin to mindful meditation, is essential to prevent the subtle shift from benign irritation to life‑threatening infection. Let us therefore honor both preventive measures and informed medical guidance, for they are the twin pillars supporting our collective wellbeing 🌟.
Pat Mills
October 13, 2025 AT 21:23Listen up, patriots! This piece finally nails the fact that our great nation cannot afford to ignore the ruthless march of respiratory foes like pneumonia and bronchitis. The shared germ army is a testament to how interconnected our health defenses must be-just as we stand united against external threats, we must also shield our lungs from bacterial invasions. The article’s emphasis on smoking as a catalyst is spot‑on; it’s the self‑inflicted wound that weakens our citizens, making them prime targets for these vicious microbes.
Now, the diagnostic arsenal-chest X‑rays, sputum tests-are the battlefield’s artillery, slicing through uncertainty and revealing the enemy’s hideouts. And don’t get me started on the treatment regime: antibiotics for bacterial pneumonia, antivirals for the flu‑driven variants, and a strict no‑antibiotic policy for viral bronchitis unless we’re certain of a superinfection. This precise approach is the hallmark of American medical excellence, cutting through the chaos with decisive action!
Our healthcare heroes must also champion vaccination, because a well‑vaccinated populace is the ultimate shield against the flu that seeds both bronchitis and pneumonia. In short, the article captures the essence of our fight: vigilance, proper diagnostics, and targeted therapy. Stay alert, stay vaccinated, and let’s keep our lungs as strong as our resolve!
Ravikumar Padala
October 13, 2025 AT 21:40Honestly, the write‑up does a decent job of laying out the basics, but let’s unpack the real-world vibe. When bronchitis lingers, the airway lining gets irritated, and that’s the perfect launch pad for germs to dive deeper into the alveoli-essentially turning a mild cough into a full‑blown pneumonia escapade. The risk factors listed, especially smoking and compromised immunity, are the usual suspects that turn a simple cold into a dangerous cascade.
From a diagnostic angle, I appreciate the reminder that a clean chest X‑ray usually points to bronchitis, while infiltrates scream pneumonia. The sputum culture is the unsung hero, actually pinpointing the pathogen and guiding antibiotic stewardship. It’s crucial because overprescribing antibiotics for viral bronchitis fuels resistance, which is a bigger nightmare than the infection itself.
Therapeutically, the split between supportive care for bronchitis-hydration, rest, bronchodilators-and targeted antibiotics for bacterial pneumonia makes perfect sense. The article also nudges us toward preventive measures: flu shots, pneumococcal vaccines, and quitting smoking. Those are the pillars that keep the transition from bronchitis to pneumonia at bay.
All in all, while the piece is a solid primer, real clinicians need to stay sharp, watch for that sudden spike in fever or chest pain, and act fast before the infection migrates deeper into the lungs.
King Shayne I
October 13, 2025 AT 21:57I think the article missed the point about how smoking actually damages your cilia and makes it way easier for germs to deep dive into your lungs. Also, they could have stressed more on the fact that a lot of people ignore mild coughs till they become serious. The whole "just rest and hydrate" line can be misleading for high‑risk folks, especially those with chronic COPD who need more aggressive monitoring. Not everything can be boiled down to "just get a vaccine"-there's a lot of nuance in diagnosing like blood work and pulse oximetry that they left out. Honestly, the piece seems a bit too generic for people who actually need detailed guidance.
jennifer jackson
October 13, 2025 AT 22:13Great info, stay healthy!
Brenda Martinez
October 13, 2025 AT 22:30You sound like you think the article nailed everything, but let’s be real-this “one‑size‑fits‑all” approach is dangerous. The dramatic flair about vaccines and X‑rays ignores the gritty reality that many patients lack access to timely imaging, leading to misdiagnosis and overtreatment. And your claim that antibiotics are always the answer for bacterial pneumonia? That’s a tired trope. Overuse breeds superbugs, turning a curable infection into a nightmare. Also, the way you glorify “high‑risk” patients as if they’re doomed to pneumonia is a fatalistic narrative that disempowers them from proactive management. We need nuanced, patient‑centered strategies, not sweeping generalizations that scare people into panic.
Marlene Schanz
October 13, 2025 AT 22:47Interesting points, Claire. I’d add that while the philosophical framing is beautiful, practical steps matter most for most readers. For instance, emphasizing the role of regular hand‑washing and avoiding crowded indoor spaces during flu season can dramatically cut down both bronchitis and pneumonia risk. Also, for chronic bronchitis patients, incorporating pulmonary rehab exercises can strengthen airway clearance, reducing the chance of bacterial migration. Lastly, reminding folks to schedule their pneumococcal vaccine well before the winter months gives the immune system a head‑start. These actionable tips bridge the gap between big ideas and daily health routines.
Matthew Ulvik
October 13, 2025 AT 23:03Hey King, I get your frustration, but don’t forget that even aggressive smokers can benefit from quitting-it's never too late. A simple step like using nicotine patches can improve ciliary function over time, making it harder for germs to stick around. Also, a quick tip: keep a pulse oximeter at home if you have chronic bronchitis; spotting a dip below 92% early can prompt a doctor visit before pneumonia sets in. Stay safe and keep an eye on those symptoms! :)
Dharmendra Singh
October 13, 2025 AT 23:20In many communities, especially where access to quick diagnostics is limited, the line between bronchitis and pneumonia can blur, leading to delayed treatment. It’s crucial to educate patients about warning signs such as sudden high fever, sharp chest pain, or rapid breathing, which may indicate a progression. Moreover, cultural practices like using traditional herbal inhalants can offer symptomatic relief, but they should complement-not replace-formal medical evaluation. Encouraging regular health check‑ups and making low‑cost chest X‑ray services available can bridge the gap and save lives.
Rocco Abel
October 13, 2025 AT 23:37Brenda, while your dramatic flair is entertaining, let’s not ignore the larger picture: pharmaceutical companies often push antibiotics as the go‑to solution, feeding a hidden agenda that keeps us dependent on costly meds. The real conspiratorial thread lies in how health data is manipulated to downplay the rise of resistant strains. In truth, the best defense is a skeptical approach to overprescription and a focus on natural immunity boosters-a perspective the mainstream media conveniently omits.