Neuropathic pain doesn’t feel like a cut or a sprain. It’s burning, electric, stabbing - sometimes even numbness that hurts. About 1 in 10 people live with it, often from diabetes, shingles, or chemo. And for many, the go-to treatments are gabapentin and pregabalin. Both are old drugs with new relevance. But they’re not the same. Choosing between them isn’t about which is "better" - it’s about which fits your life, body, and budget.
How Gabapentin and Pregabalin Work
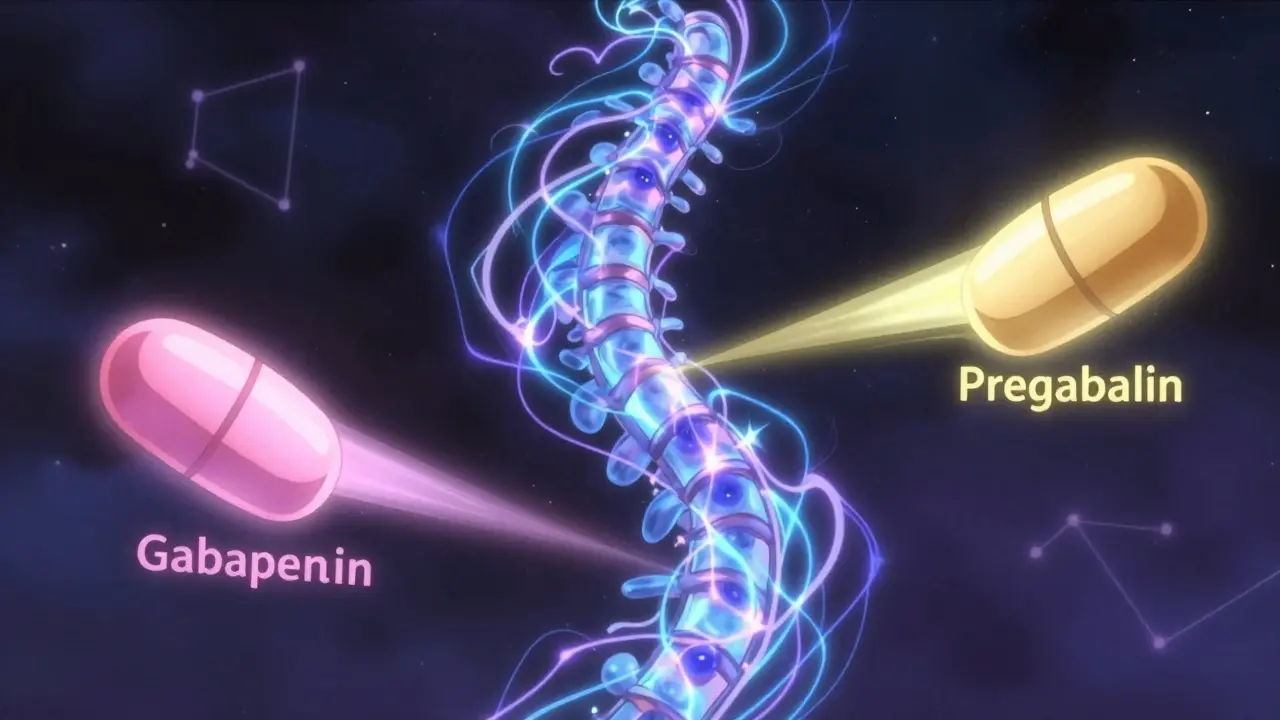
Neither drug is a painkiller like ibuprofen or opioids. They don’t block pain signals at the site of injury. Instead, they calm overactive nerves. Both bind to a specific part of nerve cells called the α2δ subunit. This reduces the flood of chemicals - like glutamate and substance P - that make nerves scream when they shouldn’t.
Here’s the twist: pregabalin binds to this spot about six times more tightly than gabapentin. That’s not just chemistry - it translates to real differences in how fast and how well they work. Pregabalin also stops the α2δ protein from moving to the spinal cord, which may help reduce nerve sensitivity over time. Gabapentin doesn’t do that.
And despite sounding like they’re related to GABA (the brain’s calming neurotransmitter), neither drug actually activates GABA receptors. That’s why they don’t cause the same sedation as benzodiazepines - though they can still make you drowsy.
Key Differences: Absorption, Dosing, and Predictability
Think of gabapentin like a leaky bucket. The more you pour in, the more leaks you get. At 900 mg a day, your body absorbs about 60%. At 3,600 mg? That drops to 33%. That’s why doubling your dose doesn’t double your relief. It just increases side effects.
Pregabalin? No leaks. It absorbs over 90% no matter the dose. That means your doctor can predict exactly how much will be in your blood. If you take 150 mg, you get twice the concentration as 75 mg. Simple. Clean. Predictable.
This matters because gabapentin takes 3 to 4 hours to peak in your system - and that time gets longer as your dose goes up. Pregabalin hits peak levels in under an hour, every time. If you’re in sudden, severe nerve pain after surgery or a flare-up, pregabalin can start working faster. Some patients report feeling relief within 24 hours. With gabapentin? It can take 3 to 4 days just to feel a hint of change.
Pain Relief: How Much Do They Actually Do?
Studies show that about 30 to 40% of people on pregabalin get at least half their pain reduced. For gabapentin? It’s closer to 25 to 35%. That difference might not sound huge, but for someone who’s been in pain for years, it’s the difference between sleeping through the night and counting minutes until morning.
Pregabalin keeps getting better as you increase the dose - up to 600 mg a day. Gabapentin? It plateaus around 1,800 mg. More than that doesn’t help much - but it does increase dizziness, swelling, and brain fog.
Real-world reviews back this up. On Drugs.com, both drugs have similar ratings - around 7.5 out of 10. But people who switch from gabapentin to pregabalin often say the same thing: "It just works more consistently." One Reddit user wrote: "Gabapentin helped, but I was always waiting for it to kick in. Pregabalin? It’s there when I need it. No guessing."

Side Effects: What You’re Really Signing Up For
Both drugs cause dizziness, drowsiness, weight gain, and swelling in the hands or feet. About 1 in 3 people experience dizziness with either drug. But pregabalin’s side effects tend to show up faster - and sometimes more intensely - because of how quickly it enters your bloodstream.
Weight gain is a big concern. About 27% of pregabalin users gain 5 pounds or more. For gabapentin, it’s 22%. That might not sound like much, but for someone with diabetes or heart issues, it can be a dealbreaker.
There’s also a difference in timing. Gabapentin’s longer half-life at high doses means it lingers. Many people take 900 mg at bedtime because it helps them sleep through the night. Pregabalin wears off faster. Some users report waking up at 3 a.m. with pain returning. That’s why some doctors recommend splitting pregabalin doses - 75 mg in the morning, 75 mg at night.
Dosing and Adjustments: It’s Not One-Size-Fits-All
If you have kidney problems - and many people with neuropathic pain do - dosing changes drastically. Gabapentin requires a complex formula based on your creatinine clearance. Most doctors don’t memorize it. They use charts. Pregabalin? It’s simpler: if your kidney function is below 60 mL/min, cut the dose in half. No math needed.
Starting doses matter too. Gabapentin usually begins at 300 mg once a day. Then it climbs slowly - 300 mg every few days - until you hit 900 to 3,600 mg. That’s a 2- to 4-week process. Pregabalin starts at 75 mg twice a day. Within a week, you’re often at 150 mg twice a day. Many patients reach their effective dose in under 10 days.
Speed matters. If you’re in acute pain after a procedure, waiting weeks for relief isn’t an option. That’s why specialists lean toward pregabalin. For stable, chronic pain? Gabapentin’s slower ramp-up might be easier to tolerate.
Cost: The Hidden Factor
Gabapentin is cheap. Generic versions cost as little as $5 a month. Pregabalin? Even generic versions run $100 to $200 a month. Insurance often requires prior authorization for pregabalin. Some patients report being denied coverage unless they’ve tried gabapentin first - even if they already know gabapentin didn’t work.
That’s why gabapentin still makes up 85% of gabapentinoid prescriptions in the U.S. It’s not because it’s better. It’s because it’s affordable. But if your pain is severe and gabapentin isn’t cutting it, paying more for pregabalin isn’t a luxury - it’s a medical necessity.
One patient on GoodRx said: "I switched to pregabalin after 2 years of gabapentin. My pain went from 8/10 to 3/10. My insurance denied it twice. I paid $180 out of pocket for 30 days. Worth every penny."
New Developments and What’s Coming
In 2023, the FDA approved a new extended-release version of pregabalin called Enseedo XR. It’s designed to release the drug slowly over 24 hours, reducing the peaks and valleys that cause side effects. Early trials show 22% fewer fluctuations in blood levels. That could mean less dizziness and better sleep.
Researchers at UCSF are also testing a new class of drugs that target only the pain-relieving part of the α2δ subunit - not the part linked to dizziness. In animal studies, they got pain relief without the brain fog. Human trials are expected to start in 2026.
But here’s the warning: gabapentinoids are being misused. Between 2012 and 2021, overdose deaths involving these drugs tripled. Most were combined with opioids. That’s why pregabalin now has a federal Risk Evaluation and Mitigation Strategy (REMS) - meaning pharmacies have to track it like a controlled substance. Gabapentin doesn’t have that yet - but it’s under review.
Who Gets Which Drug?
There’s no perfect answer. But here’s how most doctors decide:
- Choose pregabalin if: You need fast relief, your pain is severe or flaring, you have stable kidney function, and you can afford it - or your insurance covers it.
- Choose gabapentin if: Your pain is steady, you’re on a tight budget, you’re already taking other meds that cause drowsiness, or you need nighttime relief and don’t mind waiting a week to feel results.
Primary care doctors prescribe gabapentin more often - it’s cheaper and easier to manage. Pain specialists? They’re more likely to start with pregabalin. Why? Because they see patients who’ve already tried the cheaper option - and it didn’t work.
There’s no shame in starting with gabapentin. But if after 4 to 6 weeks you’re still in pain, don’t wait. Talk to your doctor about switching. Delaying effective treatment only makes nerve pain harder to control.
Final Thoughts: It’s Not About the Drug - It’s About You
Neuropathic pain is invisible. But it’s real. And it steals sleep, work, and joy. Gabapentin and pregabalin aren’t magic. But they’re two of the most studied, most reliable tools we have.
Don’t let cost or fear of side effects stop you from asking the right questions. Ask your doctor: "Which one is more likely to work for my type of pain?" "How fast can I expect results?" "What’s the plan if this doesn’t work?""
And if your doctor says, "Just take gabapentin first," ask why. Is it because it’s cheaper - or because it’s better for you? Your pain deserves more than a default option.

Catherine Scutt
January 8, 2026 AT 10:19Stop wasting time with the cheap stuff if it’s not working. Your pain doesn’t care about your deductible.
Darren McGuff
January 9, 2026 AT 16:24Also, the 3 a.m. pain wake-ups? Real. I thought I was crazy for waking up in agony. Turns out pregabalin’s half-life is shorter than my cat’s nap schedule. Splitting doses changed my life. Thank you for writing this.
Chris Kauwe
January 11, 2026 AT 15:13And don’t get me started on "just take gabapentin first" - that’s not clinical protocol. That’s insurance-driven eugenics.
Jerian Lewis
January 12, 2026 AT 01:32Kiruthiga Udayakumar
January 13, 2026 AT 01:04Maggie Noe
January 13, 2026 AT 20:12Also, the 3 a.m. pain? Real. I set an alarm to take my second dose at 2 a.m. No more crying in the dark.
Gregory Clayton
January 15, 2026 AT 14:41Johanna Baxter
January 15, 2026 AT 20:05Elisha Muwanga
January 16, 2026 AT 02:17Aron Veldhuizen
January 17, 2026 AT 08:39Micheal Murdoch
January 18, 2026 AT 15:26Here’s what I told my doctor: "I’ve tried gabapentin. It didn’t work. I’m not asking for a miracle. I’m asking for a chance." That’s it. No drama. No guilt. Just truth.
If you’re on gabapentin and still hurting after 6 weeks? Don’t wait. Don’t feel guilty. Ask again. And if they say no? Ask for a referral. Your body is worth more than a formulary list. You’re not a burden. You’re a person. And your pain? It’s valid.