Medication Allergy ID: Recognize, Avoid, and Manage Drug Reactions
When your body treats a medicine like an invader, it’s not just a side effect—it’s a medication allergy ID, a confirmed immune response to a drug that can range from mild rash to life-threatening shock. Also known as drug hypersensitivity, this isn’t about feeling a little dizzy or nauseous—it’s your immune system sounding the alarm, often with no warning. Unlike side effects, which are predictable and dose-related, a true medication allergy can happen the first time you take a drug—or after years of safe use. That’s why knowing your own medication allergy ID isn’t just smart—it’s life-saving.
People often confuse a drug rash, a skin reaction triggered by medication, often mistaken for a virus or food allergy with a full-blown allergy. But some rashes, like AGEP, can turn deadly fast. Others, like DRESS syndrome, show up weeks later with fever, swollen lymph nodes, and organ damage. Then there are reactions that hit the airways—swelling in the throat, trouble breathing, or sudden drops in blood pressure. These aren’t rare. Studies show nearly 5% of hospital visits for drug reactions are due to true allergies, and up to 20% of people report at least one drug allergy in their life. The problem? Many don’t know which drug caused it, or they assume they’re allergic to a whole class—like all penicillins—when it was just one specific molecule.
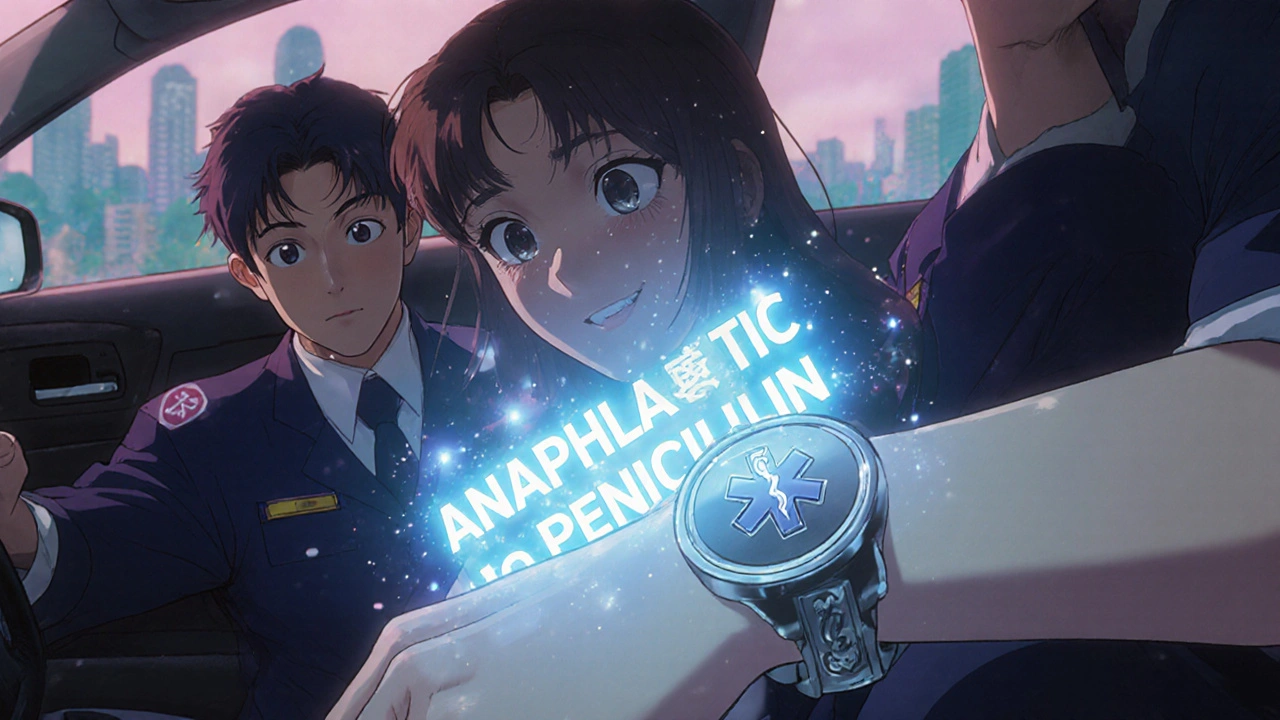
Knowing your adverse drug reaction, any harmful, unintended effect from a medication, whether allergic or not history means you can speak up in the ER, warn your pharmacist, and avoid unnecessary risks. It’s why some people carry a medical alert card or wear a bracelet. It’s why your doctor might skip certain antibiotics or painkillers even if they seem like the best choice. And it’s why post-market studies keep tracking reactions long after a drug hits shelves—because sometimes, the worst reactions only show up when thousands of people start using it.
Some drugs are more likely to trigger allergies than others. Penicillin tops the list, followed by sulfa drugs, NSAIDs like ibuprofen, and certain seizure meds. But even common OTC drugs like aspirin or antihistamines can cause reactions in the wrong person. And here’s the twist: if you’re allergic to one drug in a family, you might not be allergic to all of them. That’s why proper testing matters. Skin tests, blood tests, and controlled challenges can confirm or rule out an allergy—something most people never get.
What you’ll find in these articles isn’t just theory. You’ll see real cases—like someone who thought they were allergic to all antibiotics until testing proved otherwise, or a patient who developed a dangerous skin reaction after taking a generic version of a drug they’d used safely for years. You’ll learn how to read the fine print on labels, what to ask your doctor before starting a new med, and how to spot early signs of trouble before it’s too late. Whether you’ve had a reaction before or you’re just trying to stay safe, this collection gives you the tools to take control—not guess.
Medical Alert Bracelets: When and Why They Matter for Drug Safety
by Melissa Kopaczewski Nov 17 2025 11 MedicationsMedical alert bracelets save lives by giving emergency responders instant access to critical drug information. Learn what to engrave, which type to choose, and how to keep your info up to date for true drug safety.
READ MORE